Although derived from a colon (
large intestine)
carcinoma, when cultured under specific conditions the cells become differentiated and polarized such that their
phenotype, morphologically and functionally, resembles the
enterocytes lining the
small intestine.
[2][3] Caco-2 cells express tight junctions,
microvilli, and a number of
enzymes and transporters that are characteristic of such enterocytes:
peptidases,
esterases,
P-glycoprotein, uptake transporters for
amino acids, bile acids,
carboxylic acids, etc.
When looking at Caco-2 cell cultures microscopically, it is evident even by visual inspection that the cells are heterogeneous. As a result, over the years the characteristics of the cells used in different laboratories around the world have diverged significantly, which makes it difficult to compare results across labs.
[4]
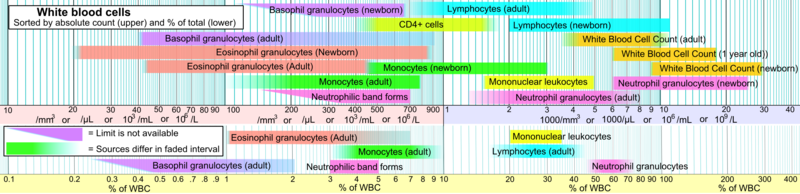
Caco-2 cells are most commonly used not as individual cells, but as a confluent
monolayer on a cell culture insert filter (e.g., Transwell). When cultured in this format, the cells differentiate to form a polarized epithelial cell monolayer that provides a physical and biochemical barrier to the passage of ions and small molecules.
[3][5] The Caco-2 monolayer is widely used across the pharmaceutical industry as an in vitro model of the human small intestinal mucosa to predict the absorption of orally administered drugs. The correlation between the in vitro apparent permeability (P¬app) across Caco-2 monolayers and the in vivo fraction absorbed (fa) is well established.
[6]Transwell diagram
This application of Caco-2 cells was pioneered in the late 1980s by Ismael Hidalgo, working in the laboratory of Ron Borchardt at the University of Kansas, and Tom Raub, who was at the
Upjohn Company at the time. Following stints at
SmithKline Beecham and
Rhone-Poulenc Rorer, Hidalgo went on to co-found a company,
Absorption Systems, in 1996, where he remains as Chief Scientist.
The considerable impact of the Caco-2 cell monolayer model can be measured in at least two ways. First, considering that poor
pharmacokinetic properties accounted for ~40% of drug failures in development in the early 1990s and only ~10% by 2009, an interval in which Caco-2 monolayers were widely used throughout the
pharmaceutical industry to predict absorption, it is not unreasonable to attribute some of that shift to this simple yet powerful model. Second, the 1989 Gastroenterology paper that demonstrated the utility of the model for this application has been cited more than 1000 times since its publication.
The versatility of Caco-2 cells is demonstrated by the fact that, even to this day, they are serving as the basis for the creation of innovative new models that are contributing to our understanding of drug efflux transporters such as P-glycoprotein (ABCB1) and BCRP (ABCG2). RNA interference has been used to silence the expression of individual efflux transporters, either transiently
[7] or long-term.
[8][9]