Thalidomide, sold under the brand name
Immunoprin, among others, is an
immunomodulatory drug and the prototype of the
thalidomide class of drugs. Today, thalidomide is used mainly as a treatment of certain cancers (
multiple myeloma) and of a complication of
leprosy. It can be readily synthesized to yield large quantities of the drug in just two steps.
Thalidomide was first marketed in 1957 in West Germany under the trade-name
Contergan. The German drug company
Chemie Grünenthal developed and sold the drug. Primarily prescribed as a
sedative or
hypnotic, thalidomide also claimed to cure "
anxiety,
insomnia,
gastritis, and tension".
[3] Afterwards, it was used against
nausea and to alleviate
morning sickness in pregnant women. Thalidomide became an
over-the-counter drug in West Germany on October 1, 1957. Shortly after the drug was sold in West Germany, between 5,000 and 7,000 infants were born with
phocomelia (malformation of the limbs). Only 40% of these children survived.
[4] Throughout the world, about 10,000 cases were reported of infants with phocomelia due to thalidomide; only 50% of the 10,000 survived. Those subjected to thalidomide while in the womb experienced limb deficiencies in a way that the long limbs either were not developed or presented themselves as stumps. Other effects included deformed eyes and hearts, deformed alimentary and urinary tracts, blindness and deafness.
[5] The negative effects of thalidomide led to the development of more structured drug regulations and control over drug use and development.
[6]
Medical uses[edit]

Pack of thalidomide capsules
There is no conclusive evidence that thalidomide or
lenalidomide is useful to bring about or maintain remission in Crohn's disease.
[10][11]
Adverse effects[edit]
Adverse effects by frequency:[12][13] Very common (may affect more than 1 in 10 people):
Common (may affect up to 1 in 10 people):
- Pulmonary embolism
- Vomiting
- Dry mouth
- Toxic skin eruption
- Dry skin
- Rash
- Urticaria (hives)
- Pyrexia (fever)
- Asthenia
- Interstitial lung disease
- Heart failure
- Depression
- Pneumonia
Uncommon (may affect up to 1 in 100 people):
- Shortness of breath
- Tremor
Rare (may affect up to 1 in 1,000 people):
- Increased appetite
- Bradycardia (low heart rate)
- Tachycardia (high heart rate)
- Cardiac arrhythmia
- Malaise
- Deep vein thrombosis
Very rare (may affect up to 1 in 10,000 people):
† Peripheral neuropathy may be irreversible and usually results from chronic (usually a matter of months) exposure to thalidomide.
[13]
Carcinogenicity[edit]
Animal studies did not demonstrate any
carcinogenicity even when rats and mice were exposed to up to 11 times the therapeutic dose of thalidomide.
[14] Despite this there have been some concerns that it may cause secondary malignancies in patients with multiple myeloma. The FDA has issued a statement that it is investigating these concerns.
[15]
Some clinical trials have supported this claim and the major secondary malignancy that thalidomide is associated with is
acute myeloid leukaemia.
[16] The
MHRA of the
UK and
Health Canada of
Canada have also issued warnings to healthcare professionals regarding the risk of secondary malignancies due to thalidomide exposure.
[17][18]
Contraindications[edit]
Contraindications include:
[14]
- Known hypersensitivity to thalidomide
- Pregnancy or breastfeeding
- Patient age < 12 years
- Patients who are unable or unwilling to comply with required contraceptive measures
Interactions[edit]
There are no expected
pharmacokinetic interactions between thalidomide and other medicines due to its neutral effects on p-glycoprotein and P450 cytochromes.
[14] It may interact with sedatives due to its sedative action.
[14] It may also interact with bradycardic agents due to its bradycardia-inducing effects.
[14] The risk of peripheral neuropathy may be increased by concomitant treatment with other agents known to cause peripheral neuropathy.
[14] The risk of venous thromboembolisms with thalidomide seems to be increased when patients are treated with oral contraceptives or other cytotoxic agents (including doxorubicin and melphalan) concurrently.
[14]Thalidomide may interfere with the contraceptive effects of various contraceptives and hence it is advised that women of reproductive age use at least two different means of contraception to ensure that no child will be conceived while they are receiving thalidomide.
[14]
Overdose[edit]
Eighteen cases of overdoses have been reported to date with doses of up to 14.4 g without any reported fatalities.
[14] No specific antidote for overdoses exists and treatment is purely supportive.
[14]
Pharmacology[edit]
The precise mechanism of action for thalidomide is unknown; efforts to identify thalidomide's
teratogenic action generated 2000 research papers and the proposal of 15 or 16 plausible mechanisms by 2000.,
[19] As of 2015 the main theories were inhibition of the process of
angiogenesis, its inhibition of
cereblon, a
ubiquitin ligase, and its ability to generate
reactive oxygen species which in turn kill cells.
[20][21]
Chemistry[edit]

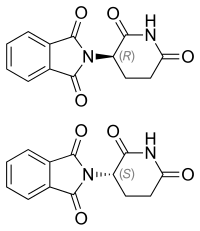
The two enantiomers of thalidomide:
Left: (
S)-(−)-thalidomide
Right: (
R)-(+)-thalidomide
Thalidomide is
racemic; while the S-thalidomide is the bioactive form of the molecule, the individual enantiomers can
racemize to each other due to the acidic hydrogen at the
chiral centre, which is the carbon of the glutarimide ring bonded to the phthalimide substituent. The racemization process can occur
in vivo.
[2][24][25][26]
Celgene Corporation originally synthesized thalidomide using a three-step sequence starting with
L-glutamic acid treatment, but this has since been reformed by the use of
L-glutamine.
[27] As shown in the image below, N-carbethoxyphtalimide (1) can react with L-glutamine to yield N-Phthaloyl-L-glutamine (2). Cyclization of N-Phthaloyl-L-glutamine occurs using
carbonyldiimidazole, which then yields thalidomide (3).
[27] Celegne Corporation's original method resulted in a 31% yield of S-thalidomide, whereas the two-step synthesis yields 85-93% product that is 99% pure.

Muller et al.'s two-step thalidomide synthesis
History[edit]
Thalidomide was
discovered by scientists at the German pharmaceutical company
Chemie Grünenthal (now
Grünenthal GmbH) around 1953. The company had been set up as a soap maker just after WWII ended, to address the urgent market need for antibiotics. Heinrich Mueckter, was appointed to head the discovery program based on his experience working with the German army's antiviral research program. In the course of preparing
reagents for the work, Mueckter's assistant Wilhelm Kunz isolated a by-product, that was in turn recognized by pharmacologist Herbert Keller as an analog of
glutethimide, a
sedative, and the medicinal chemistry work turned to improving the lead compound into a suitable drug; the result was thalidomide. The toxicity was examined in several animals, and the drug was introduced in 1956 as a sedative.
[28]
Researchers at
Chemie Grünenthal also found that thalidomide was a particularly effective
antiemetic that had an inhibitory effect on
morning sickness.
[29] Hence, on October 1, 1957, the company launched thalidomide and began aggressively marketing it under the trade name
Contergan.
[30][better source needed] It was proclaimed a "wonder drug" for
insomnia, coughs, colds and headaches.
[citation needed]
During this time period, the use of medications during pregnancy was not strictly controlled, and drugs were not thoroughly tested for potential harm to the
fetus.
[29]Thousands of pregnant women took the drug to relieve their symptoms. At the time of the drug's development, scientists did not believe any drug taken by a pregnant woman could pass across the
placental barrier and harm the developing fetus,
[6] even though the effect of alcohol on fetal development had been documented by case studies on alcoholic mothers since at least 1957.
[31] There soon appeared reports of findings of abnormalities in children being born, traced back to the use of the drug thalidomide. In late 1959, it was noticed that
peripheral neuritis developed in patients who took the drug over a period of time, and it was only after this point that thalidomide ceased to be provided over the counter.
[32]
Hence, while initially considered safe, the drug was responsible for
teratogenic deformities in children born after their mothers used it during pregnancies, prior to the third trimester. In November 1961, thalidomide was taken off the market due to massive pressure from the press and public.
[33] Experts estimate that the drug thalidomide led to the death of approximately 2,000 children and serious birth defects in more than 10,000 children, about 5,000 of them in
West Germany.
[citation needed] The regulatory authorities in
East Germany did not approve thalidomide.
[4][dead link] One reason for the initially unobserved side effects of the drug and the subsequent approval in West Germany was that at that time drugs did not have to be tested for
teratogenic effects. They had been tested on rodents only, as was usual at the time.
[34]
In the UK, the British pharmaceutical company
The Distillers Company (Biochemicals) Ltd, a subsidiary of
Distillers Co. Ltd. (now part of
Diageo plc), marketed thalidomide under the brand name
Distaval as a remedy for
morning sickness throughout the United Kingdom, Australia and New Zealand. Their advertisement claimed that "Distaval can be given with complete safety to pregnant women and nursing mothers without adverse effect on mother or child...Outstandingly safe Distaval has been prescribed for nearly three years in this country."
[4][dead link] Around the world, more and more pharmaceutical companies started to produce and market the drug under license from
Chemie Grünenthal. By the mid 1950s, 14 pharmaceutical companies were marketing thalidomide in 46 countries under 37 (some reports suggest 51) different trade names.
In the U.S., representatives from
Chemie Grünenthal approached
Smith, Kline & French (SKF), now
GlaxoSmithKline (GSK) with a request to market and distribute the drug in North America. A memorandum rediscovered in 2010 in the archives of the U.S.
Food and Drug Administration (FDA) shows that, as part of its in-licensing approach,
Smith, Kline and French conducted animal tests and ran a clinical trial of the drug in the United States involving 875 people, including pregnant women, in 1956–57.
[citation needed] In 1956, researchers at SKF involved in clinical trials noted that even when used in very high doses, thalidomide could not induce sleep in mice.
[citation needed] And when administered at doses 50 to 650 times larger than that claimed by
Chemie Grünenthal to be "sleep inducing", the researchers could still not achieve the hypnotic effect in animals that it had on humans.
[citation needed] After completion of the trial, and based on reasons kept hidden for decades, SKF declined to commercialize the drug. Later,
Chemie Grünenthal, in 1958, reached an agreement with
William S Merrell Company in Cincinnati, Ohio, (
later Richardson-Merrell, now part of
Sanofi), to market and distribute thalidomide throughout the United States.
[4][dead link]
The U.S. FDA refused to approve thalidomide for marketing and distribution. However, the drug was distributed in large quantities for testing purposes, after the American distributor and manufacturer
Richardson-Merrell had applied for its approval in September 1960.
[citation needed] The official in charge of the FDA review,
Frances Oldham Kelsey, did not rely on information from the company, which did not include any test results. Richardson-Merrell was called on to perform tests and report the results. The company demanded approval six times, and was refused each time. Nevertheless, a total of 17 children with thalidomide-induced malformations were born in the U.S.
[35]
In Canada, the history of the drug thalidomide dates back to April 1, 1961. There were many different forms sold, with the most common variant being Talimol.
[36] Two months after Talimol went on sale, pharmaceutical companies sent physicians letters warning about the risk of birth defects.
[36] It was not until March 2, 1962, that both drugs were banned from the Canadian market by the FDD, and soon afterward physicians were warned to destroy their supplies.
[36]
Leprosy treatment[edit]
In 1964, Israeli physician
Jacob Sheskin administered thalidomide to a patient critically ill with leprosy. The patient exhibited
erythema nodosum leprosum (ENL), a painful skin condition, one of the complications of
leprosy. This was attempted despite the ban on thalidomide's use, but results were favourable: the patient slept for hours and was able to get out of bed without aid upon awakening. A clinical trial studying the use of thalidomide in leprosy soon followed.
[37]
Thalidomide has been used by Brazilian physicians as the drug of choice for the treatment of severe ENL since 1965, and by 1996, at least 33 cases of thalidomide embryopathy were recorded in people born in Brazil after 1965.
[38] Since 1994, the production, dispensing, and prescription of thalidomide have been strictly controlled, requiring women to use two forms of birth control and submit to regular pregnancy tests. Despite this, cases of thalidomide embryopathy continue,
[39][40] with at least 100 cases identified in Brazil between 2005 and 2010.
[41] 5.8 million thalidomide pills were distributed throughout Brazil in this time period, largely to poor Brazilians in areas with poor access to healthcare, and these cases have occurred despite the controls.
In 1998 the FDA approved the drug's use in the treatment of ENL.
[42] Because of thalidomide's potential for causing birth defects, the drug may be distributed only under tightly controlled conditions. The FDA required that
Celgene Corporation, which planned to market thalidomide under the brand name
Thalomid, establish a system for thalidomide education and prescribing safety (STEPS) oversight program. The conditions required under the program include limiting prescription and dispensing rights to authorized prescribers and pharmacies only, keeping a registry of all patients prescribed thalidomide, providing extensive patient education about the risks associated with the drug, and providing periodic pregnancy tests for women who take the drug.
[42]
Cancer treatment[edit]
Shortly after the teratogenic properties of thalidomide were recognized in the mid-1960s, its anti-cancer potential was explored and two clinical trials were conducted in people with advanced cancer, including some people with multiple myeloma; the trials were inconclusive.
[44]
Little further work was done with thalidomide in cancer until the 1990s.
[44]
Judah Folkman pioneered studies into the role of
angiogenesis (the proliferation and growth of blood vessels) in the development of cancer, and in the early 1970s had shown that
solid tumors could not expand without it.
[45][46] In 1993 he surprised the scientific world by hypothesizing the same was true of
blood cancers,
[47] and the next year he published work showing that a
biomarker of angiogenesis was higher in all people with cancer, but especially high in people with blood cancers, and other evidence emerged as well.
[47] Meanwhile, a member of his lab, Robert D'Amato, was looking for
angiogenesis inhibitors, and discovered in 1994 that thalidomide inhibited angiogenesis.
[48] Around that time, the wife of a man who was dying of multiple myeloma and whom standard treatments had failed, called Folkman asking him about his anti-angiogenesis ideas.
[46] Folkman convinced the patient's doctor to try thalidomide, and that doctor conducted a clinical trial of thalidomide for people with multiple myeloma in which about a third of the subjects responded to the treatment.
[46] The results of that trial were published in the New England Journal of Medicine in 1999.
[46][49]
After further work was done by Celgene and others, in 2006 the U.S. Food and Drug Administration granted accelerated approval for thalidomide in combination with dexamethasone for the treatment of newly diagnosed
multiple myeloma patients.
[46][50]
Society and culture[edit]
Regulatory approved uses[edit]
Birth defects crisis[edit]

Baby born to a mother who had taken thalidomide while pregnant
In the late 1950s and early 1960s, more than 10,000 children in 46 countries were born with
deformities such as
phocomelia as a consequence of thalidomide use.
[58] The severity and location of the deformities depended on how many days into the pregnancy the mother was before beginning treatment; thalidomide taken on the 20th day of pregnancy caused central brain damage, day 21 would damage the eyes, day 22 the ears and face, day 24 the arms, and leg damage would occur if taken up to day 28. Thalidomide did not damage the foetus if taken after 42 days gestation.
[33]
It is not known exactly how many worldwide victims of the drug there have been, although estimates range from 10,000 to 20,000
[59] to 100,000.
[33] Despite the side effects, thalidomide was sold in pharmacies in Canada until 1962.
[36][60]
In the United Kingdom, the drug was licensed in 1958 and withdrawn in 1961. Of the approximately 2,000 babies born with defects, around half died within a few months and 466 survived to at least 2010.
[61]
In Spain, thalidomide was widely available throughout the 1970s, perhaps even into the 1980s. There were two reasons for this. First, state controls and safeguarding were poor; indeed, it was not until 2008 that the government even admitted the country had ever imported thalidomide. Second, Grünenthal failed to insist that its sister company in Madrid warn Spanish doctors, and permitted it to not warn them. The Spanish advocacy group for victims of thalidomide estimates that in 2015, there were 250–300 living victims of thalidomide in Spain.
[62]
The Australian obstetrician
William McBride and the German
paediatrician Widukind Lenz suspected a link between birth defects and the drug, a theory Lenz proved in 1961.
[63][64] McBride was later awarded a number of honors, including a medal and prize money by L'Institut de la Vie in Paris.
[65] Further animal tests were conducted by Dr George Somers, Chief Pharmacologist of
Distillers Company in Britain, which showed foetal abnormalities in rabbits.
[66] Similar results were also published showing these effects in rats
[67][68] and other species.
[69]
In
East Germany, the head of the central pharmacy control commission, Friedrich Jung, suspected an antivitaminic effect of thalidomide as derivative of
glutamic acid.
[70] Meanwhile, in
West Germany, it took some time before the increase in
dysmelia at the end of the 1950s was connected with thalidomide. In 1958 Karl Beck, a former pediatric doctor in
Bayreuth wrote an article in a local newspaper claiming a relationship between nuclear weapons testing and cases of dysmelia in children.
[71]Based on this,
FDP whip Erich Mende requested an official statement from the federal government.
[71] For statistical reasons, the main data series used to research dysmelia cases started by chance at the same time as the approval date for thalidomide.
[71] After the Nazi regime with its
Law for the Prevention of Hereditarily Diseased Offspring used mandatory statistical monitoring to commit various
crimes, western Germany had been very reluctant to monitor
congenital disorders in a similarly strict way.
[72] The parliamentary report rejected any relation with radioactivity and the abnormal increase of dysmelia.
[71] Also the DFG research project installed after the Mende request was not helpful. The project was led by pathologist
Franz Büchner who ran the project to propagate his
teratological theory. Büchner saw lack of healthy nutrition and behavior of the mothers as being more important than genetic reasons.
[72] Furthermore, it took a while to install a Surgeon General in Germany; the
Federal Ministry of Health (Germany) was not founded until 1962, some months after thalidomide was banned from the market.
[71] In Germany approximately 2,500 thalidomide babies were born.
[64]
Several countries either restricted the drug's use or never approved it. Ingeborg Eichler, a member of the
Austrian pharmaceutical admission conference, enforced thalidomide (tradename Softenon) being sold under the rules of
prescription medication and as a result relatively few affected children were born in Austria and Switzerland.
[73] In the United States,
pharmacologist Frances Oldham Kelsey M.D. withstood pressure from the
Richardson-Merrell company and refused
Food and Drug Administration (FDA) approval to market thalidomide, saying further studies were needed.
[58] This reduced the impact of thalidomide in United States patients. Although thalidomide was never approved for sale in the United States at the time, millions of tablets had been distributed to physicians during a clinical testing program. It was impossible to know how many pregnant women had been given the drug to help alleviate morning sickness or as a sedative.
[74]
Aftermath of scandal[edit]
The numerous reports of malformations in babies brought about the awareness of the side effects of the drug on pregnant women. The birth defects caused by the drug thalidomide can range from moderate malformation to more severe forms. Possible birth defects include phocomelia, dysmelia, amelia, bone hypoplasticity, and other congenital defects affecting the ear, heart, or internal organs.
[29] Franks et al. looked at how the drug affected newborn babies, the severity of their deformities, and reviewed the drug in its early years. Webb in 1963 also reviewed the history of the drug and the different forms of birth defects it had caused. "The most common form of birth defects from thalidomide is shortened limbs, with the arms being more frequently affected. This syndrome is the presence of deformities of the long bones of the limbs resulting in shortening and other abnormalities."
[36]
Germany[edit]
In 1968, a large criminal trial began in Germany, charging several Grünenthal officials with negligent homicide and injury. After Grünenthal settled with the victims in April 1970, the trial ended in December 1970 with no finding of guilt. As part of the settlement, Grünenthal paid 100 million
DM into a special foundation; the German government added 320 million DM. The foundation paid victims a one-time sum of 2,500-25,000 DM (depending on severity of disability) and a monthly stipend of 100-450 DM. The monthly stipends have since been raised substantially and are now paid entirely by the government (as the foundation had run out of money). Grünenthal paid another 50 million Euros into the foundation in 2008.
On 31 August 2012, Grünenthal chief executive Harald F. Stock, PhD, who served as the Chief Executive Officer of Grünenthal GmbH from January 2009 to May 28, 2013 and was also a Member of Executive Board until May 28, 2013, apologized for the first time for producing the drug and remaining silent about the birth defects.
[75]At a ceremony, Stock unveiled a statue of a disabled child to symbolize those harmed by thalidomide and apologized for not trying to reach out to victims for over 50 years. At the time of the apology, there were 5,000 to 6,000 sufferers still alive. Victim advocates called the apology "insulting" and "too little, too late", and criticized the company for not compensating victims. They also criticized the company for their claim that no one could have known the harm the drug caused, arguing that there were plenty of red flags at the time.
[76]
United Kingdom[edit]
In 1968, after a long campaign by
The Sunday Times, a compensation settlement for the UK victims was reached with
Distillers Company (now part of
Diageo), which had distributed the drug in the UK.
[77][78] This compensation, which is distributed by the Thalidomide Trust in the UK, was substantially increased by Diageo in 2005.
[79]The UK Government gave survivors a grant of £20 million, to be distributed through the Thalidomide Trust, in December 2009.
[80]
Australia[edit]
Melbourne woman Lynette Rowe, who was born without limbs, led an Australian
class action lawsuit against the drug's manufacturer, Grünenthal, which fought to have the case heard in Germany. The
Supreme Court of Victoria dismissed Grünenthal's application in 2012, and the case was heard in Australia.
[81] On 17 July 2012, Rowe was awarded an out-of-court settlement, believed to be in the millions of dollars and paving the way for class action victims to receive further compensation.
[82] In February 2014, the Supreme Court of Victoria endorsed the settlement of $89 million AUD to 107 victims of the drug in Australia and New Zealand.
[83][84]
The drug thalidomide's birth defects in children affected many people's lives, and from these events came the formation of the group called
The Thalidomide Victims Association of Canada, a group of 120 Canadian survivors.
[85][86] Their goal was to prevent future usage of drugs that could be of potential harm to mothers and babies. The members from the thalidomide victims association were involved in the STEPS program, which aimed to prevent teratogenicity.
[29]
The effects of thalidomide increased fears regarding the safety of pharmaceutical drugs. The Society of Toxicology of Canada was formed after the effects of thalidomide were made public, focusing on toxicology as a discipline separate from pharmacology.
[87] The need for the testing and approval of the toxins in certain pharmaceutical drugs became more important after the disaster. The Society of Toxicology of Canada is responsible for the Conservation Environment Protection Act, focusing on researching the impact to human health of chemical substances.
[87] Thalidomide brought on changes in the way drugs are tested, what type of drugs are used during pregnancy, and increased the awareness of potential side effects of drugs.
United States[edit]
For correctly denying the application despite the pressure from Richardson-Merrell, Kelsey eventually received the President's Award for Distinguished Federal Civilian Service at a 1962 ceremony with President
John F. Kennedy. In September 2010, the FDA honored Kelsey with the first Kelsey award. The award, given annually to an FDA staff member, came 50 years after Kelsey, then a new medical officer at the agency, first reviewed the application from the William S. Merrell Company of Cincinnati.
[89] Cardiologist
Helen B. Taussig learned of the damaging effects of the drug thalidomide on newborns and in 1967, testified before Congress on this matter after a trip to Germany where she worked with infants with
phocomelia (severe limb deformities). As a result of her efforts, thalidomide was banned in the United States and Europe.
[citation needed]
Notable cases[edit]

Niko von Glasow, German filmmaker
- Lorraine Mercer MBE of the United Kingdom, born with phocomelia of both arms and legs, is the only thalidomide survivor to carry the Olympic Torch.[90]
- Thomas Quasthoff, an internationally acclaimed bass-baritone, who describes himself: "1.34 meters tall, short arms, seven fingers — four right, three left — large, relatively well-formed head, brown eyes, distinctive lips; profession: singer".[91]
- Niko von Glasow produced a documentary called NoBody's Perfect, based on the lives of 12 people affected by the drug, which was released in 2008.[92][93]
- Mercédes Benegbi, born with phocomelia of both arms, drove the successful campaign for compensation from her government for Canadians who were affected by thalidomide.[94]
Change in drug regulations[edit]
Research[edit]
Research efforts have been focused on determination how thalidomide causes birth defects and its other activities in the human body, efforts to develop safer analogs, and efforts to find further uses for thalidomide.
Thalidomide analogs[edit]
The exploration of the
antiangiogenic and immunomodulatory activities of thalidomide has led to the study and creation of thalidomide
analogs.
[99][100] Celgene has sponsored numerous clinical trials with analogues to thalidomide, such as
lenalidomide, that are substantially more powerful and have fewer side effects — except for greater
myelosuppression.
[101] In 2005, Celgene received FDA approval for
lenalidomide (Revlimid) as the first commercially useful derivative. Revlimid is available only in a restricted distribution setting to avoid its use during pregnancy. Further studies are being conducted to find safer compounds with useful qualities. Another more potent analog,
pomalidomide, is now FDA approved.
[102] Additionally,
apremilast was approved by the FDA in March 2014. These
thalidomide analogs can be used to treat different diseases, or used in a regimen to fight two conditions.
[103]