TRAIL and Taurolidine Enhance the Anticancer Activity of Doxorubicin .
Doxorubicin và Trabectedin kháng HT1080
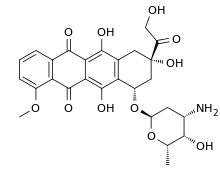
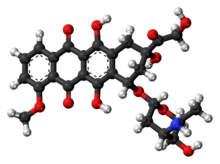
Doxorubicin
From Wikipedia, the free encyclopedia
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌdɒksəˈruːbᵻsɪn/ |
| Trade names | Adriamycin, Doxil, Caelyx, Myocet, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682221 |
| Pregnancy category | |
| Routes of administration | intravenous, intravesical |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 5% (by mouth) |
| Protein binding | 75%[1] |
| Metabolism | Liver |
| Biological half-life | Triphasic; 12 minutes, 3.3 hours, 30 hours. Mean: 1-3 hours[1][2] |
| Excretion | Urine (5-12%), faeces (40-50%)[1] |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.041.344 |
| Chemical and physical data | |
| Formula | C27H29NO11 |
| Molar mass | 543.52 g/mol |
| 3D model (Jmol) | |
| | |
Doxorubicin, sold under the trade names Adriamycin among others, is a chemotherapy medication used to treat cancer. This includes breast cancer, bladder cancer, Kaposi's sarcoma, lymphoma, and acute lymphocytic leukemia. It is often used together with other chemotherapy agents. Doxorubicin is given by injection into a vein.[3]
Common side effects include hair loss, bone marrow suppression, vomiting, rash, and inflammation of the mouth. Other serious side effects may include allergic reactions such as anaphylaxis, heart damage, tissue damage at the site of injection, radiation recall, and treatment-related leukemia. People often experience red discoloration of the urine for a few days. Doxorubicin is in the anthracycline and antitumor antibiotic family of medications.[3] It works in part by interfering with the function of DNA.[4]
Doxorubicin was approved for medical use in the United States in 1974.[3] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[5] The wholesale cost in the developing world is about 3.88 to 32.79 USD per 50 mg vial.[6] In the United Kingdom this amount costs the NHS about £100.12.[7][8] Versions that are pegylated and in liposomes are also available; however, are more expensive.[8]Doxorubicin was originally made from the bacteria Streptomyces peucetius.[9]
Contents
[hide]Medical use[edit]
Doxorubicin is commonly used to treat some leukemias and Hodgkin's lymphoma, as well as cancers of the bladder, breast, stomach, lung, ovaries, thyroid, soft tissue sarcoma, multiple myeloma, and others.[2][10] Commonly used doxorubicin-containing regimens are AC (adriamycin, cyclophosphamide), TAC (taxotere, AC), ABVD (Adriamycin, bleomycin, vinblastine, dacarbazine), BEACOPP, CHOP (cyclophosphamide, hydroxydaunorubicin, vincristine, prednisone) and FAC (5-fluorouracil, adriamycin, cyclophosphamide).[2]
Doxil (see below) is used primarily for the treatment of ovarian cancer where the disease has progressed or recurred after platinum-based chemotherapy, or for the treatment of AIDS-related Kaposi's sarcoma.[11]
Liposomal form[edit]
There is a pegylated (polyethylene glycol coated) liposome-encapsulated form of doxorubicin, sold as Doxil. It was developed to treat Kaposi's sarcoma, an AIDS-related cancer that causes lesions to grow under the skin, in the lining of the mouth, nose and throat, or in other organs. The polyethylene glycol coating results in preferential concentration of doxorubicin in the skin. However, this also results in a side effect called palmar plantar erythrodysesthesia (PPE), more commonly known as hand-foot syndrome. Following administration of this form of doxorubicin, small amounts of the drug can leak from capillaries in the palms of the hands and soles of the feet. The result of this leakage is redness, tenderness, and peeling of the skin that can be uncomfortable and even painful. In clinical testing at 50 mg/m2 dosing every 4 weeks, half of people developed hand-foot syndrome. The rate of this side effect limits the dose of this formulation that can be given as compared with plain doxorubicin in the same treatment regimen, thereby limiting potential substitution. Substitution would be desirable because liposome-encapsulated doxorubicin is less cardiotoxic than unencapsulated doxorubicin. This form is also approved by the FDA for treatment of ovarian cancer and multiple myeloma.[12][13]
A non-pegylated liposomal doxorubicin, called Myocet, is approved in Europe and Canada for treatment of metastatic breast cancer in combination with cyclophosphamide, but has not been approved by the FDA for use in the United States. Unlike Doxil, the Myocet liposome does not have a polyethylene glycol coating, and therefore does not result in the same rate of hand-foot syndrome. The minimization of this side effect may allow for one for one substitution with doxorubicin in the same treatment regimen, thereby improving safety with no loss of efficacy. Like Doxil, the liposomal encapsulation of the doxorubicin limits the cardiotoxicity. In theory, by limiting the cardiotoxicity of doxorubicin through liposomal encapsulation, it can be used safely in concurrent combination with other cardiotoxic chemotherapy drugs, such as trastuzumab. There is an FDA black box warning that trastuzumab cannot be used in concurrent combination with doxorubicin, only in sequential combination. Though concurrent combination of trastuzumab and doxorubicin in clinical studies found superior tumor response, the combination resulted in unacceptable cardiotoxicity, including risk of cardiac failure manifesting as congestive heart failure (CHF). Published phase II study results have shown that Myocet, trastuzumab, and paclitaxel can safely be used concurrently without the cardiac risk, as measured by reduction in LVEF function, while still achieving superior tumor response. This finding is the basis for the ongoing phase III trial for FDA approval.[12]
Side effects[edit]
The most dangerous side effect of doxorubicin is cardiomyopathy, leading to congestive heart failure. The rate of cardiomyopathy is dependent on its cumulative dose, with an incidence about 4% when the dose of doxorubicin is 500–550 mg/m², 18% when the dose is 551–600 mg/m² and 36% when the dose exceeds 600 mg/m².[14]There are several ways in which doxorubicin is believed to cause cardiomyopathy, including oxidative stress, downregulation of genes for contractile proteins, and p53mediated apoptosis.[14] The drug dexrazoxane is used to mitigate doxorubicin's cardiotoxicity.
Another common and potentially fatal complication of doxorubicin is typhlitis, an acute life-threatening infection of the bowel.[15]
Additionally, some patients may develop PPE, characterized by skin eruptions on the palms of the hand or soles of the feet, swelling, pain, and erythema.[11]
Due to these side effects and its red color, doxorubicin has earned the nickname "red devil"[16] or "red death."[17]
Chemotherapy can cause reactivation of hepatitis B, and doxorubicin-containing regimens are no exception.[18][19]
Doxorubicin and several chemotherapeutic drugs (including cyclophosphamide) cause dyspigmentation. Other groups of drugs that cause this problem include antimalarials, amiodarone, heavy metals (but not iron), tetracyclines, and antipsychotics.[20]
Biosynthesis[edit]
Doxorubicin (DXR) is a 14-hydroxylated version of daunorubicin, the immediate precursor of DXR in its biosynthetic pathway. Daunorubicin is more abundantly found as a natural product because it is produced by a number of different wild type strains of Streptomyces. In contrast, only one known non-wild type species, Streptomyces peucetius subspecies cesius ATCC 27952, was initially found to be capable of producing the more widely used doxorubicin.[21] This strain was created by Arcamone et al. in 1969 by mutating a strain producing daunorubicin, but not DXR, at least in detectable quantities.[22] Subsequently, Hutchinson's group showed that under special environmental conditions, or by the introduction of genetic modifications, other strains of Streptomyces can produce doxorubicin.[23] His group has also cloned many of the genes required for DXR production, although not all of them have been fully characterized. In 1996, Strohl's group discovered, isolated and characterized dox A, the gene encoding the enzyme that converts daunorubicin into DXR.[24] By 1999, they produced recombinant dox A, a cytochrome P450 oxidase, and found that it catalyzes multiple steps in DXR biosynthesis, including steps leading to daunorubicin.[25] This was significant because it became clear that all daunorubicin-producing strains have the necessary genes to produce DXR, the much more therapeutically important of the two. Hutchinson's group went on to develop methods to improve the yield of DXR, from the fermentation process used in its commercial production, not only by introducing dox A encoding plasmids, but also by introducing mutations to deactivate enzymes that shunt DXR precursors to less useful products, for example baumycin-like glycosides.[21] Some triple mutants, that also over-expressed dox A, were able to double the yield of DXR. This is of more than academic interest, because at that time DXR cost about $1.37 million per kg and current production in 1999 was 225 kg per annum.[26] More efficient production techniques have brought the price down to $1.1 million per kg for the nonliposomal formulation. Although DXR can be produced semi-synthetically from daunorubicin, the process involves electrophilic bromination and multiple steps, and the yield is poor.[27] Since daunorubicin is produced by fermentation, it would be ideal if the bacteria could complete DXR synthesis more effectively.
Mechanism of action[edit]
Doxorubicin interacts with DNA by intercalation and inhibition of macromolecular biosynthesis.[4][29][30] This inhibits the progression of topoisomerase II, an enzyme which relaxes supercoils in DNA for transcription.[31] Doxorubicin stabilizes the topoisomerase II complex after it has broken the DNA chain for replication, preventing the DNA double helix from being resealed and thereby stopping the process of replication.[4] It may also increase quinone type free radical production, hence contributing to its cytotoxicity.[10]
The planar aromatic chromophore portion of the molecule intercalates between two base pairs of the DNA, while the six-membered daunosamine sugar sits in the minor groove and interacts with flanking base pairs immediately adjacent to the intercalation site, as evidenced by several crystal structures.[28][32]
By intercalation, doxorubicin can also induce histone eviction from transcriptionally active chromatin.[33][34] As a result, DNA damage response, epigenome and transcriptome are deregulated in doxorubicin-exposed cells.[33]
History[edit]
In the 1950s, an Italian research company, Farmitalia Research Laboratories, began an organized effort to find anticancer compounds from soil-based microbes. A soil sample was isolated from the area surrounding the Castel del Monte, a 13th-century castle. A new strain of Streptomyces peucetius, which produced a red pigment, was isolated, and an antibiotic from this bacterium was effective against tumors in mice. Since a group of French researchers discovered the same compound at about the same time, the two teams named the compound daunorubicin, combining the name Dauni, a pre-Roman tribe that occupied the area of Italy where the compound was isolated, with the French word for ruby, rubis, describing the color.[35][36][37] Clinical trials began in the 1960s, and the drug was successful in treating acute leukemia and lymphoma. However, by 1967, it was recognized that daunorubicin could produce fatal cardiac toxicity.[38]
Researchers at Farmitalia soon discovered that changes in biological activity could be made by minor changes in the structure of the compound. A strain of Streptomyces was mutated using N-nitroso-N-methyl urethane, and this new strain produced a different, red-colored antibiotic. They named this new compound Adriamycin, after the Adriatic Sea, and the name was later changed to doxorubicin to conform to the established naming convention.[22] Doxorubicin showed better activity than daunorubicin against mouse tumors, and especially solid tumors. It also showed a higher therapeutic index, yet the cardiotoxicity remained.[39]
Doxorubicin and daunorubicin together can be thought of as prototype compounds for the anthracyclines. Subsequent research has led to many other anthracycline antibiotics, or analogs, and there are now over 2,000 known analogs of doxorubicin. By 1991, 553 of them had been evaluated in the screening program at the National Cancer Institute (NCI).[35] In 2016 GPX-150 was granted orphan drug designation by US FDA.[40]
Society and culture[edit]
Names[edit]
It is also known as hydroxydaunorubicin and hydroxydaunomycin.
It is sold under a number of different brand names, including Adriamycin PFS, Adriamycin RDF, or Rubex.[2]
Formulations[edit]
Doxorubicin is photosensitive, and containers are often covered by an aluminum bag and/or brown wax paper to prevent light from affecting it.[2] Doxorubicin is also available in liposome-encapsulated forms as Doxil (pegylated form), Myocet (nonpegylated form), and Caelyx, although these forms must also be given by intravenous injection.[2]
Shortage[edit]
As of February 2014, Doxil was available in limited supply.[41] In 2011, Doxil became available only in very limited supply due to production problems with the third-party manufacturer. Johnson & Johnson (JNJ), through its subsidiary Janssen Products, LP, had been receiving its Doxil supply from contract manufacturer Ben Venue Laboratories (located in Bedford, Ohio), a unit of Boehringer Ingelheim GmbH of Germany.[42] The problems began when Ben Venue temporarily shut down their manufacturing facility due to quality control issues.[43]
In February 2012, to address the Doxil shortage, the US Food and Drug Administration (FDA) allowed for the temporary importation of Lipodox, which contains the same active ingredient as Doxil and is made by Sun Pharma Global FZE (Sun), a subsidiary of India's Sun Pharmaceutical Industries Ltd.[44] The agency said it intends to continue allowing the importation of Lipodox until Sun has made enough generic Doxil to meet demand.[45]
The FDA approved the first generic version of Doxil, made by Sun, in February 2013. It will be available in 20 milligram and 50 milligram vials.[46]
Research[edit]
Combination therapy experiments with sirolimus (rapamycin) and doxorubicin have shown promise in treating Akt-positive lymphomas in mice.[47]
Recent animal research coupling a murine monoclonal antibody with doxorubicin has created an immunoconjugate that was able to eliminate HIV-1 infection in mice. Current treatment with antiretroviral therapy (ART) still leaves pockets of HIV within the host. The immunoconjugate could potentially provide a complementary treatment to ART to eradicate antigen-expressing T cells.[48]
Antimalarial activity[edit]
There is some evidence for antimalarial activity for doxorubicin and similar compounds. In 2009, a compound similar in structure to doxorubicin was found to inhibit plasmepsin II, an enzyme unique to the malarial parasite Plasmodium falciparum.[49] The pharmaceutical company GlaxoSmithKline (GSK) later identified doxorubicin in a set of compounds that inhibit parasite growth [50]
Fluorescence[edit]
Doxorubicin is also known to be fluorescent. This has often been used to characterize doxorubicin concentrations, and has opened the possibility of using the molecule as a theranostic agent. However, there are significant limitations, as doxorubicin's fluorescence spectrum is known to depend on a variety of factors, including the pH of the environment, solvent dielectric constant and others. Doxorubicin fluorescence is quenched by binding to DNA, and shielded by micelle encapsulation. It is also known to self-quench at high concentrations. In contrast, histone binding amplifies fluorescence.[51][52]
Trabectedin
From Wikipedia, the free encyclopedia
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| License data | |
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Not applicable (IV only) |
| Protein binding | 94 to 98% |
| Metabolism | Hepatic (mostly CYP3A4-mediated) |
| Biological half-life | 180 hours (mean) |
| Excretion | Mostly fecal |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.223.368 |
| Chemical and physical data | |
| Formula | C39H43N3O11S |
| Molar mass | 761.84 g/mol |
| 3D model (Jmol) | |
| | |
Trabectedin (also known as ecteinascidin 743 or ET-743) is an anti-tumor drug. It is sold by Pharma Mar S.A. and Johnson and Johnson under the brand name Yondelis. It is approved for use in Europe, Russia and South Korea for the treatment of advanced soft tissue sarcoma. It is also undergoing clinical trials for the treatment of breast, prostate, and paediatric sarcomas. The European Commission and the U.S. Food and Drug Administration (FDA) have granted orphan drug status to trabectedin for soft tissue sarcomas and ovarian cancer.
Contents
[hide]Discovery and production[edit]
During the 1950s and 1960s, the National Cancer Institute carried out a wide ranging program of screening plant and marine organism material. As part of that program extract from the sea squirt Ecteinascidia turbinata was found to have anticancer activity in 1969.[1] Separation and characterisation of the active molecules had to wait many years for the development of sufficiently sensitive techniques, and the structure of one of them, Ecteinascidin 743, was determined by KL Rinehart at the University of Illinois in 1984.[2] Rinehart had collected his sea squirts by scuba diving in the reefs of the West Indies.[3] Recently, the biosynthetic pathway responsible for producing the drug has been determined to come from Candidatus Endoecteinascidia frumentensis, a microbial symbiont of the tunicate.[4] The Spanish company PharmaMarlicensed the compound from the University of Illinois before 1994[citation needed] and attempted to farm the sea squirt with limited success.[3] Yields from the sea squirt are extremely low - it takes 1 tonne of animals to isolate 1 gram of trabectedin - and about 5 grams were believed to be needed for a clinical trial[5] so Rinehart asked the Harvard chemist E. J. Corey to search for a synthetic method of preparation. His group developed such a method and published it in 1996.[6]This was later followed by a simpler and more tractable method which was patented by Harvard and subsequently licensed to PharmaMar.[3] The current supply is based on a semisynthetic process developed by PharmaMar starting from safracin B, an antibiotic obtained by fermentation of the bacterium Pseudomonas fluorescens.[7] PharmaMar have entered into an agreement with Johnson & Johnson to market the compound outside Europe.[citation needed]
Approvals and indications[edit]
Trabectedin was first trialed in humans in 1996.[citation needed]
Soft tissue sarcoma[edit]
In 2007, the EMEA gave authorization for the marketing of trabectedin, under the trade name Yondelis, for the treatment of patients with advanced soft tissue sarcoma, after failure of anthracyclines and ifosfamide, or who are unsuited to receive these agents. The agency's evaluating committee, the CHMP, observed that trabectedin had not been evaluated in an adequately designed and analyzed randomized trial against current best care, and that the clinical efficacy data was mainly based on patients with liposarcoma and leiomyosarcoma. However the pivotal study did show a significant difference between two different trabectedin treatment regimens, and due to the rarity of the disease the CHMP considered that marketing authorisation could be granted under exceptional circumstances.[8] As part of the approval PharmaMar agreed to conduct a further trial to identify whether any specific chromosomal translocations could be used to predict responsiveness to trabectedin.[9]
Trabectedin is also approved in South Korea[10] and Russia.
In 2015 (after phase III study comparing with dacarbazine[11]) the US FDA approved trabectedin (Yondelis) for the treatment of liposarcoma and leiomyosarcoma that is either unresectable or has metastasized. Patients must have received prior chemotherapy with an anthracycline.[12]
Ovarian cancer and other[edit]
In 2008 the submission was announced of a registration dossier to the European Medicines Agency (EMEA) and the FDA for Yondelis when administered in combination with pegylated liposomal doxorubicin (Doxil, Caelyx) for the treatment of women with relapsed ovarian cancer. In 2011, Johnson&Johnson voluntarily withdrew the submission in the United States following a request by the FDA for an additional Phase III study to be done in support of the submission.[13]
Structure[edit]
Trabectedin is composed of 3 tetrahydroisoquinoline moieties, 8 rings including one 10-membered heterocyclic ring containing a cysteine residue, and 7 chiral centers.
Biosynthesis[edit]
The biosynthesis of trabectedin in Candidatus Endoecteinascidia frumentensis starts with a fatty acid loading onto the acyl-ligase domain of the EtuA3 module. A cysteine and glycine are then loaded as canonical NRPS amino acids. A tyrosine residue is modified by the enzymes EtuH, EtuM1, and EtuM2 to add a hydroxyl at the meta position of the phenol, and adding two methyl groups at the para-hydroxyl and the meta carbon position. This modified tyrosine reacts with the original substrate via a Pictet-Spengler reaction, where the amine group is converted to an imine by deprotonation, then attacks the free aldehyde to form a carbocation that is quenched by electrons from the methyl-phenol ring. This is done in the EtuA2 T-domain. This reaction is done a second time to yeid a dimer of modified tyrosine residues that have been further cyclized via Pictet-Spengler reaction, yielding a bicyclic ring moiety. The EtuO and EtuF3 enzymes continue to post-translationally modify the molecule, adding several functional groups and making a sulfide bridge between the original cysteine residue and the beta-carbon of the first tyrosine to form ET-583, ET-597, ET-596, and ET-594 which have been previously isolated.[4] A third O-methylated tyrosine is added and cyclized via Pictet-Spangler to yield the final product.[4]
Total synthesis[edit]
The total synthesis by E.J. Corey [6] used this proposed biosynthesis to guide their synthetic strategy. The synthesis uses such reactions as the Mannich reaction, Pictet-Spengler reaction, the Curtius rearrangement, and chiral rhodium-based diphosphine-catalyzed enantioselective hydrogenation. A separate synthetic process also involved the Ugi reaction to assist in the formation of the pentacyclic core. This reaction was unprecedented for using such a one pot multi-component reaction in the synthesis of such a complex molecule.
Mechanism of action[edit]
Recently, it has been shown that Trabectedin blocks DNA binding of the oncogenic transcription factor FUS-CHOP and reverses the transcriptional program in myxoid liposarcoma. By reversing the genetic program created by this transcription factor, Trabectedin promotes differentiation and reverses the oncogenic phenotype in these cells.[15]
Other than transcriptional interference, the mechanism of action of Trabectedin is complex and not completely understood. The compound is known to bind and alkylate DNA at the N2 position of guanine. It is known from in-vitro work that this binding occurs in the minor groove, spans approximately 3 to 5 bp and is most efficient with CGG sequences. Additional favorable binding sequences are TGG, AGC, or GGC. Once bound, this reversible covalent adduct bends DNA toward the major groove, interferes directly with activated transcription, poisons the transcription-coupled nucleotide excision repair (TCR) complex, promotes degradation of RNA polymerase II, and generates DNA double-strand breaks.[15]


No comments:
Post a Comment