Gallium maltolate kháng HCC
From Wikipedia, the free encyclopedia
 | |
| Names | |
|---|---|
| IUPAC name
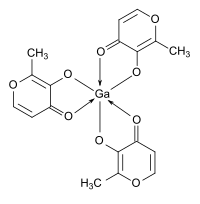
Tris(3-hydroxy-2-methyl-4H-pyran-4-one)gallium
| |
| Identifiers | |
| UNII | |
| Properties | |
| Ga(C6H5O3)3 | |
| Molar mass | 445.03 g/mol |
| Appearance | White to pale beige crystalline solid or powder |
| Density | 1.56 g/cm3, solid |
| Melting point | 220 °C (decomposes) |
| 24(2) mM; 10.7(9) mg/mL (25 °C) | |
| Structure | |
| Orthorhombic; space groupPbca | |
| Distorted octahedral | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
| Infobox references | |
Gallium maltolate is a coordination complex consisting of a trivalent gallium cation coordinated to three maltolateligands. The compound is undergoing clinical and preclinical testing as a potential therapeutic agent for cancer, infectious disease, and inflammatory disease.[1][2][3][4] It appears to have low toxicity when administered orally, without the renal toxicity observed for intravenously administered gallium nitrate. The lower toxicity probably results because gallium absorbed into the body from oral gallium maltolate becomes nearly entirely protein bound, whereas gallium from intravenous gallium nitrate tends to form anionic gallium hydroxide (Ga(OH)4−; gallate) in the blood, which is rapidly excreted in the urine and may be renally toxic.[1] A cosmetic skin cream containing gallium maltolate is marketed under the name Gallixa.
Contents
[hide]Chemical properties[edit]
In aqueous solutions, gallium maltolate has neutral charge and pH, and is stable between about pH 5 and 8. It has significant solubility in both water and lipids (octanol:water partition coefficient = 0.41).[1]
Research and pharmaceutical development[edit]
Pharmaceutical compositions and uses of gallium maltolate were first patented by Lawrence R. Bernstein.[5][6][7][8][9][10]
Christopher Chitambar and his associates at the Medical College of Wisconsin have found that gallium maltolate is active against several lymphoma cell lines, including those resistant to gallium nitrate.[3]
Gallium maltolate is able to deliver gallium with high oral bioavailability: the bioavailability is several times higher than that of gallium salts such as gallium nitrate and gallium trichloride.[1] In vitro studies have found gallium to be antiproliferative due primarily to its ability to mimic ferric iron (Fe3+). Ferric iron is essential for DNA synthesis, as it is present in the active site of the enzyme ribonucleotide reductase, which catalyzes the conversion of ribonucleotides to the deoxyribonucleotides required for DNA. Gallium is taken up by the rapidly proliferating cells, but it is not functional for DNA synthesis, so the cells cannot reproduce and they ultimately die by apoptosis. Normally reproducing cells take up little gallium (as is known from gallium scans), and gallium is not incorporated into hemoglobin, accounting for the relatively low toxicity of gallium.[11]
Gallium has been repeatedly shown to have anti-inflammatory activity in animal models of inflammatory disease.[2][11][12]Orally administered gallium maltolate has demonstrated efficacy against two types of induced inflammatory arthritis in rats.[12] Experimental evidence suggests that the anti-inflammatory activity of gallium may be due, at least in part, to down-regulation of pro-inflammatory T-cells and inhibition of inflammatory cytokine secretion by macrophages.[2][11][12] Because many iron compounds are pro-inflammatory, the ability of gallium to act as a non-functional iron mimic may contribute to its anti-inflammatory activity.[2]
Gallium maltolate is being studied as a potential treatment for primary liver cancer (hepatocellular carcinoma; HCC). In vitro experiments demonstrated efficacy against HCC cell lines[4] and one clinical case report produced encouraging results.[13]
The activity of gallium against infection-related biofilms, particularly those caused by Pseudomonas aeruginosa, is being studied by Pradeep Singh at the University of Washington, and by others, who have reported encouraging results in mice.[14][15] Pulmonary P. aeruginosa biofilms are responsible for many fatalities in cystic fibrosis and immunocompromised patients; in general, bacterial biofilms are responsible for significant morbidity and mortality.[16] In related research, locally administered gallium maltolate has shown potent efficacy against P. aeruginosa in a mouse burn/infection model.[17]
Oral gallium maltolate is also being investigated as a treatment for Rhodococcus equi foal pneumonia, a common and often fatal disease of newborn horses. R. equican also infect humans with AIDS or who are otherwise immunocompromized. The veterinary studies are being conducted by researchers at Texas A&M University, led by Ronald Martens, Noah Cohen, and M. Keith Chaffin.[18][19]
Topically applied gallium maltolate has been studied in case reports for use in neuropathic pain (severe postherpetic neuralgia and trigeminal neuralgia).[12] It has been hypothesized that any effect on pain may be related to gallium's anti-inflammatory mechanisms, and possibly from its interactions with certain matrix metalloproteinasesand substance P, whose activities are zinc-mediated and which have been implicated in the etiology of pain.[12]
