Glutathione[1]
 |
 |
| Names |
|---|
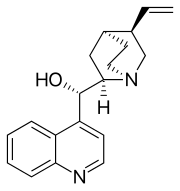
IUPAC name
(2S)-2-Amino-4-{[(1R)-1-[(carboxymethyl)carbamoyl]-2-sulfanylethyl]carbamoyl}butanoic acid
|
Other names
γ-L-Glutamyl-L-cysteinylglycine
(2S)-2-Amino-5-[[(2R)-1-(carboxymethylamino)-1-oxo-3-sulfanylpropan-2-yl]amino]-5-oxopentanoic acid
|
| Identifiers |
|---|
|
|
|
|
|
|
| Abbreviations | GSH |
| ChEBI |
|
| ChemSpider |
|
| DrugBank |
|
| ECHA InfoCard | 100.000.660 |
|
|
|
| KEGG |
|
| MeSH | Glutathione |
|
|
|
| UNII |
|
InChI=1S/C10H17N3O6S/c11-5(10(18)19)1-2-7(14)13-6(4-20)9(17)12-3-8(15)16/h5-6,20H,1-4,11H2,(H,12,17)(H,13,14)(H,15,16)(H,18,19)/t5-,6-/m0/s1 
Key: RWSXRVCMGQZWBV-WDSKDSINSA-N 
InChI=1/C10H17N3O6S/c11-5(10(18)19)1-2-7(14)13-6(4-20)9(17)12-3-8(15)16/h5-6,20H,1-4,11H2,(H,12,17)(H,13,14)(H,15,16)(H,18,19)/t5-,6-/m0/s1
Key: RWSXRVCMGQZWBV-WDSKDSINBK
|
C(CC(=O)N[C@@H](CS)C(=O)NCC(=O)O)[C@@H](C(=O)O)N
|
| Properties |
|---|
|
| C10H17N3O6S |
| Molar mass | 307.32 g·mol−1 |
| Melting point | 195 °C (383 °F; 468 K) |
|
| Freely soluble[1] |
| Solubility in methanol, diethyl ether | Insoluble |
| Pharmacology |
|---|
|
| V03AB32 (WHO) |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
|
 verify (what is verify (what is   ?) ?) |
| Infobox references |
| |
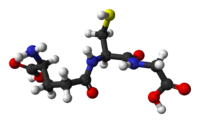
Once oxidized, glutathione can be reduced back by glutathione reductase, using
NADPH as an electron donor.
[3] The ratio of reduced glutathione to oxidized glutathione within cells is often used as a measure of cellular
oxidative stress.
[4][5]
Biosynthesis[edit]
Glutathione is not an
essential nutrient for humans, since it can be synthesized in the body from the
amino acids L-cysteine,
L-glutamic acid, and
glycine; it does not have to be present as a supplement in the diet. The
sulfhydryl group (SH) of cysteine serves as a
proton donor and is responsible for its biological activity. Cysteine is the rate-limiting factor in cellular glutathione biosynthesis, since this amino acid is relatively rare in foods.
- First, gamma-glutamylcysteine is synthesized from L-glutamate and cysteine via the enzyme gamma-glutamylcysteine synthetase (glutamate cysteine ligase, GCL). This reaction is the rate-limiting step in glutathione synthesis.[8]
- Second, glycine is added to the C-terminal of gamma-glutamylcysteine via the enzyme glutathione synthetase.
Animal
glutamate cysteine ligase (GCL) is a
heterodimeric enzyme composed of a catalytic and a modulatory subunit. The catalytic subunit is necessary and sufficient for all GCL enzymatic activity, whereas the modulatory subunit increases the catalytic efficiency of the enzyme. Mice lacking the catalytic subunit (i.e., lacking all
de novo GSH synthesis) die before birth.
[9] Mice lacking the modulatory subunit demonstrate no obvious phenotype, but exhibit marked decrease in GSH and increased sensitivity to toxic insults.
[10][11][12]
While all animal cells are capable of synthesizing glutathione, glutathione synthesis in the liver has been shown to be essential. GCLC
knockout mice die within a month of birth due to the absence of hepatic GSH synthesis.
[13][14] Major transport into the blood stream is driven by an
electrochemical gradient, specifically through the
transport proteins RcGshT and RsGshT.
[15] Similarly, glutathione
S-conjugates, synthesized hepatically, feature preferential secretion into
bile.
[14][16]
The plant
glutamate cysteine ligase (GCL) is a redox-sensitive
homodimeric enzyme, conserved in the plant kingdom.
[17] In an oxidizing environment, intermolecular disulfide bridges are formed and the enzyme switches to the dimeric active state. The midpoint potential of the critical cysteine pair is -318 mV. In addition to the redox-dependent control, the plant GCL enzyme is feedback inhibited by glutathione.
[18] GCL is exclusively located in
plastids, and
glutathione synthetase (GS) is dual-targeted to plastids and cytosol, thus GSH and
gamma-glutamylcysteine are exported from the plastids.
[19] Both glutathione biosynthesis enzymes are essential in plants; knock-outs of GCL and GS are lethal to embryo and seedling.
[20]
Function[edit]
Glutathione exists in both reduced (GSH) and oxidized (
GSSG) states. In the reduced state, the thiol group of cysteine is able to donate a
reducing equivalent (H
++ e
−) to other molecules, such as reactive oxygen species to neutralize them, or to protein cysteines to maintain their reduced forms. With donating an electron, glutathione itself becomes reactive and readily reacts with another reactive glutathione to form
glutathione disulfide (GSSG). Such a reaction is probable due to the relatively high concentration of glutathione in cells (up to 7 mM in the liver).
[21]
Generally, interactions between GSH and other molecules with higher relative
electrophilicity deplete GSH levels within the cell. An exception to this case involves the sensitivity of GSH to the electrophilic compound's relative concentration. In high concentrations, the organic molecule
Diethyl maleate fully depleted GSH levels in cells. However, in low concentrations, a minor decrease in cellular GSH levels was followed by a two-fold increase.
[22][23]
GSH can be regenerated from GSSG by the enzyme
glutathione reductase (GSR):
[3] NADPH reduces FAD present in GSR to produce a transient FADH-anion. This anion then quickly breaks a disulfide bond (Cys58 - Cys63) and leads to Cys63's nucleophilically attacking the nearest sulfide unit in the GSSG molecule (promoted by His467), which creates a mixed disulfide bond (GS-Cys58) and a GS-anion. His467 of GSR then protonates the GS-anion to form the first GSH. Next, Cys63 nucleophilically attacks the sulfide of Cys58, releasing a GS-anion, which, in turn, picks up a solvent proton and is released from the enzyme, thereby creating the second GSH. So, for every GSSG and NADPH, two reduced GSH molecules are gained, which can again act as antioxidants scavenging reactive oxygen species in the cell.
In healthy cells and tissue, more than 90% of the total glutathione pool is in the reduced form (GSH) and less than 10% exists in the disulfide form (GSSG). An increased GSSG-to-GSH ratio is considered indicative of
oxidative stress.
[24]
Glutathione has multiple functions:
- It maintains levels of reduced glutaredoxin and glutathione peroxidase[25]
- It is one of the major endogenous antioxidants produced by the cells, participating directly in the neutralization of free radicals and reactive oxygen compounds, as well as maintaining exogenous antioxidants such as vitamins C and E in their reduced (active) forms.[26][27][28]
- Regulation of the nitric oxide cycle is critical for life, but can be problematic if unregulated.[29]
- It is used in metabolic and biochemical reactions such as DNA synthesis and repair, protein synthesis, prostaglandin synthesis, amino acid transport, and enzyme activation. Thus, every system in the body can be affected by the state of the glutathione system, especially the immune system, the nervous system, the gastrointestinal system, and the lungs.[citation needed]
- It has a vital function in iron metabolism. Yeast cells depleted of GSH or containing toxic levels of GSH show an intense iron starvation-like response and impairment of the activity of extramitochondrial ISC enzymes thus inhibiting oxidative endoplasmic reticulum folding, followed by death.[30]
- It has roles in progression of the cell cycle, including cell death.[5] GSH levels regulate redox changes to nuclear proteins necessary for the initiation of cell differentiation. Differences in GSH levels also determine the expressed mode of cell death, being either apoptosis or cell necrosis. Manageably low levels result in the systematic breakage of the cell whereas excessively low levels result in rapid cell death.[31]
Function in animals[edit]
In the case of
N-acetyl-p-benzoquinone imine (NAPQI), the reactive
cytochrome P450-reactive
metabolite formed by
paracetamol (acetaminophen), which becomes toxic when GSH is depleted by an overdose of acetaminophen, glutathione is an essential antidote to overdose. Glutathione conjugates to NAPQI and helps to detoxify it. In this capacity, it protects cellular protein thiol groups, which would otherwise become covalently modified; when all GSH has been spent, NAPQI begins to react with the cellular
proteins, killing the cells in the process. The preferred treatment for an overdose of this painkiller is the administration (usually in atomized form) of
N-acetyl-L-cysteine (often as a preparation called Mucomyst
[32]), which is processed by cells to
L-cysteine and used in the
de novo synthesis of GSH.
This detoxification reaction is carried out by the
glyoxalase system.
Glyoxalase I (EC 4.4.1.5) catalyzes the conversion of methylglyoxal and reduced glutathione to
S-
D-lactoyl-glutathione.
Glyoxalase II (EC 3.1.2.6) catalyzes the hydrolysis of
S-
D-lactoyl-glutathione to glutathione and
D-lactic acid.
Function in plants[edit]
Supplementation[edit]
Calcitriol (1,25-dihydroxyvitamin D
3), the active metabolite of
vitamin D3, after being synthesized from
calcifediol in the kidney, increases glutathione levels in the brain and appears to be a catalyst for glutathione production.
[43] It takes about ten days for the body to process vitamin D
3 into calcitriol.
[44]
S-adenosylmethionine (SAMe), a cosubstrate involved in methyl group transfer, has also been shown to increase cellular glutathione content in persons suffering from a disease-related glutathione deficiency.
[45][46][47]
Low glutathione is commonly observed in wasting and negative nitrogen balance, as seen in cancer, HIV/AIDS,
sepsis, trauma, burns, and athletic overtraining. Low levels are also observed in periods of starvation. These effects are hypothesized to be influenced by the higher glycolytic activity associated with
cachexia, which result from reduced levels of oxidative phosphorylation.
[48][49]
Bioavailability[edit]
Systemic
bioavailability of orally consumed glutathione is poor because the molecule, a tripeptide, is the substrate of
proteases (peptidases) of the alimentary canal, and due to the absence of a specific
carrier of glutathione at the level of cell membrane.
[50][51]
Methods to determine glutathione[edit]
Small molecule based glutathione probes[edit]
Ellman's reagent and Monobromobimane[edit]
Reduced glutathione may be visualized using
Ellman's reagent or
bimane derivatives such as
monobromobimane. The monobromobimane method is more sensitive. In this procedure, cells are lysed and thiols extracted using a
HCl buffer. The thiols are then reduced with
dithiothreitol and labelled by monobromobimane. Monobromobimane becomes fluorescent after binding to GSH. The thiols are then separated by
HPLC and the fluorescence quantified with a fluorescence detector.
Monochlorobimane[edit]
Monochlorobimane can be used to quantify glutathione
in vivo. The quantification is done by
confocal laser scanning microscopy after application of the dye to living cells.
[52] This quantification process relies on measuring the rates of fluorescence changes and is limited to plant cells.
5-Chloromethylfluorescein diacetate (CMFDA)[edit]
CMFDA was initially used as a cell tracker. Unfortunately, it has also been mistakenly used as a glutathione probe. Unlike monochlorobimane, whose fluorescence increases upon reacting with glutathione, the fluorescence increase of CMFDA is due to the hydrolysis of the acetate groups inside cells. Although CMFDA may react with glutathione in cells, the fluorescence increase does not reflect the reaction. Therefore, studies using CMFDA as a glutathione probe should be revisited and re-interpreted.
[53][54]
ThiolQuant Green[edit]
The major limitation of these bimane based probes and many other reported probes is that these probes are based on irreversible chemical reactions with glutathione, which renders these probes incapable of monitoring the real-time glutathione dynamics. Recently, the first reversible reaction based fluorescent probe-ThiolQuant Green (TQG)-for glutathione was reported.
[55] ThiolQuant Green can not only perform high resolution measurements of glutathione levels in single cells using a confocal microscope, but also be applied in flow cytometry to perform bulk measurements.
Protein based glutathione probes[edit]
Another approach, which allows measurement of the glutathione redox potential at a high spatial and temporal resolution in living cells is based on redox imaging using the
redox-sensitive green fluorescent protein (roGFP)
[56] or redox sensitive yellow fluorescent protein (rxYFP)
[57] GSSG because its very low physiological concentration is difficult to measure accurately unless the procedure is carefully executed and monitored and the occurrence of interfering compounds is properly addressed. GSSG concentration ranges from 10 to 50 μM in all solid tissues, and from 2 to 5 μM in blood (13–33 nmol per gram Hb). GSH-to-GSSG ratio ranges from 100 to 700.
[58]
Other biological implications[edit]
The sulphur-rich aspect of glutathione results in it forming relatively strong complexes with lead(II).
[59]
Once a tumor has been established, elevated levels of glutathione may act to protect cancerous cells by conferring resistance to chemotherapeutic drugs.
[60] The antineoplastic mustard drug
canfosfamide was modelled on the structure of glutathione.
Cystic fibrosis[edit]
Several studies have been completed on the effectiveness of introducing inhaled glutathione to people with cystic fibrosis with mixed results.
[61][62]
Alzheimer's disease (AD)[edit]
Whilst extracellular
amyloid beta (Aβ) plaques,
neurofibrillary tangles (NFT), inflammation in the form of reactive
astrocytes and
microglia, and neuronal loss are all consistent pathological features of AD, a mechanistic link between these factors is yet to be clarified. Although the majority of past research has focused on fibrillar Aβ, soluble oligomeric Aβ species are now considered to be of major pathological importance in AD. Up-regulation of GSH may be protective against the oxidative and neurotoxic effects of oligomeric Aβ.
Winemaking[edit]
Cosmetics[edit]
Glutathione plays an important role in preventing
oxidative damage to the skin.
[65] In addition to its many recognized biological functions, glutathione has also been associated with skin lightening ability.
[66] The role of glutathione as a skin whitener was discovered as a side effect of large doses of glutathione.
[67] Glutathione utilizes different mechanisms to exert its action as a skin whitening agent at various levels of
melanogenesis. It inhibits
melanin synthesis by means of stopping the neurotransmitter precursor
L-DOPA’s ability to interact with
tyrosinase in the process of melanin production.
[68] Glutathione inhibits the actual production as well as
agglutination of melanin by interrupting the function of L-DOPA. Another study found that glutathione inhibits melanin formation by direct inactivation of the enzyme tyrosinase by binding and
chelating copper within the enzyme’s active site.
[69] Glutathione’s antioxidant property allows it to inhibit melanin synthesis by quenching of
free radicals and
peroxides that contribute to tyrosinase activation and melanin formation.
[70] Its antioxidant property also protects the skin from UV radiation and other environmental as well as internal stressors that generate free radicals that cause skin damage and
hyperpigmentation.
[71] In most mammals, melanin formation consists of
eumelanin (brown-black pigment) and
pheomelanin ( yellow-red pigment) as either mixtures or co-polymers.
[72] Increase in glutathione level may induce the pigment cell to produce pheomelanin instead of eumelanin pigments.
[73] A research by Te-Sheng Chang found lowest levels of reduced glutathione to be associated with eumelanin type pigmentation, whereas the highest ones were associated with the pheomelanin.
[66] As a result, it is reasonable to assume that depletion of glutathione would result in eumelanin formation. Prota
[74] observed that decreased glutathione concentration led to the conversion of
L-Dopaquinone to
Dopachrome, increasing the formation of brown-black pigment (eumelanin).
Importance of gamma-glutamylcysteine as a precursor for glutathione synthesis[edit]
Gamma-glutamylcysteine (GGC) is the immediate precursor to GSH. GGC supplementation would circumvent feedback inhibitory control of GCL by the end product GSH. Accordingly, a method of elevating GSH levels with the notable advantage of bypassing negative feedback inhibition has been described. Because of this, GGC has been the focus of therapeutic efforts since Puri and Meister 1983. The first documented use of GGC in brains appears to be Pileblad and Magnusson, 1992. Astroglia cells are capable of utilising GGC.
[75] Direct delivery of the GSH precursor GCC to brain has been reported to effectively replenish levels of GSH in the brain.
[76]
Most of the work done on GGC has been preclinical, based on in vivo animal models, or in vitro brain cultures. In order for the therapeutic value of GGC elevation against AD to be vindicated, three empirical hurdles have to be cleared. The first is to demonstrate that delivery of GCC into the brain can indeed increase GSH.
[76] The second is to demonstrate that the increase in GGC can indeed reduce oxidative stress in the brain,
[77] a condition frequently linked with cognitive decline.