Methotrexate Resistance in an L1210 Cell Line Resulting from ...
Methotrexate thuốc kháng L1210
From Wikipedia, the free encyclopedia
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | |
| Trade names | Trexall, Rheumatrex, others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682019 |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth, IV, IM, SC, intrathecal |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 60% at lower doses, less at higher doses.[5] |
| Protein binding | 35–50% (parent drug),[5] 91–93% (7-hydroxymethotrexate)[6] |
| Metabolism | Hepatic and intracellular[5] |
| Biological half-life | 3–10 hours (lower doses), 8–15 hours (higher doses)[5] |
| Excretion | Urine (80–100%), faeces (small amounts)[5][6] |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| ECHA InfoCard | 100.000.376 |
| Chemical and physical data | |
| Formula | C20H22N8O5 |
| Molar mass | 454.44 g/mol |
| 3D model (Jmol) | |
| (verify) | |
Methotrexate (MTX), formerly known as amethopterin, is a chemotherapy agent and immune system suppressant.[1] It is used to treat cancer, autoimmune diseases, ectopic pregnancy, and for medical abortions. Types of cancers it is used for include breast cancer, leukemia, lung cancer, lymphoma, and osteosarcoma. Types of autoimmune diseases it is used for include psoriasis, rheumatoid arthritis, and Crohn's disease. It can be given by mouth or by injection.[1]
Common side effects include nausea, feeling tired, fever, increased risk of infection, low white blood cell counts, and breakdown of the skin inside the mouth. Other side effects may include liver disease, lung disease, lymphoma, and severe skin rashes. People on long-term treatment should be regularly checked for side effects. It is not safe during breastfeeding. In those with kidney problems, lower doses may be needed. It acts by blocking the body's use of folic acid.[1]
Methotrexate was made in 1947 and initially came into medical use to treat cancer, as it was less toxic than the current treatments.[7] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[8] Methotrexate is available as a generic medication.[1] The wholesale cost as of 2014 in the developing world is between US$0.06 and 0.36 per day for the form taken by mouth.[9] In the United States, a typical month of treatment costs $25 to $50.[10]
Contents
[hide]Medical uses[edit]
Chemotherapy[edit]
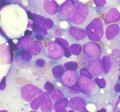
Methotrexate was originally developed and continues to be used for chemotherapy, either alone or in combination with other agents. It is effective for the treatment of a number of cancers, including: breast, head and neck, leukemia, lymphoma, lung, osteosarcoma, bladder, and trophoblastic neoplasms.[1]
Autoimmune disorders[edit]
It is used as a disease-modifying treatment for some autoimmune diseases, including rheumatoid arthritis, juvenile dermatomyositis, psoriasis, psoriatic arthritis, lupus, sarcoidosis, Crohn's disease (although a recent review has raised the point that it is fairly underused in Crohn's disease),[11] eczema and many forms of vasculitis.[12][13]Although originally designed as a chemotherapy drug (using high doses), in low doses, methotrexate is a generally safe and well tolerated drug in the treatment of certain autoimmune diseases. Because of its effectiveness, low-dose methotrexate is now first-line therapy for the treatment of rheumatoid arthritis. Weekly doses are beneficial for 12 to 52 weeks duration therapy, although discontinuation rates are as high as 16% due to adverse effects.[14] Although methotrexate for autoimmune diseases is taken in lower doses than it is for cancer, side effects such as hair loss, nausea, headaches, and skin pigmentation are still common.[12][15][16] Use of low doses of methotrexate together with NSAIDS such as aspirin or paracetamol is relatively safe in people being treated for rheumatoid arthritis, if adequate monitoring is done.[17]
Not everyone with rheumatoid arthritis responds favorably to treatment with methotrexate, but multiple studies and reviews showed that the majority of people receiving methotrexate for up to one year had less pain, functioned better, had fewer swollen and tender joints, and had less disease activity overall as reported by themselves and their doctors. X-rays also showed that the progress of the disease slowed or stopped in many people receiving methotrexate, with the progression being completely halted in about 30% of those receiving the drug.[18] Those individuals with rheumatoid arthritis treated with methotrexate have been found to have a lower risk of cardiovascular events such as myocardial infarctions (heart attacks) and strokes.[19]
Recently, use of methotrexate in combination with anti-TNF agents has been shown to be effective for the treatment of ulcerative colitis.[20]
Methotrexate has also been used for multiple sclerosis.[1]
It is not commonly used for lupus, and only tentative evidence exists to support the practice.[21]
Abortion[edit]
Methotrexate is an abortifacient and is commonly used to terminate pregnancies during the early stages, generally in combination with misoprostol. It is also used to treat ectopic pregnancies, provided the fallopian tube has not ruptured.[1][22]
Molar pregnancy[edit]
Methotrexate with dilatation and curettage is used to treat molar pregnancy.
Administration[edit]
Methotrexate can be given by mouth or by injection (intramuscular, intravenous, subcutaneous, or intrathecal).[1] Doses by mouth are usually taken weekly, not daily, to limit toxicity.[1] Routine monitoring of the complete blood count, liver function tests, and creatinine are recommended.[1] Measurements of creatinine are recommended at least every 2 months.[1]
Adverse effects[edit]
The most common adverse effects include: hepatotoxicity (liver damage), ulcerative stomatitis, leukopenia and thus predisposition to infection, nausea, abdominal pain, fatigue, fever, dizziness, acute pneumonitis, rarely pulmonary fibrosis, and kidney failure.[12][1] Methotrexate is teratogenic (harmful to a fetus) and hence is not advised for either the prospective father to take it before or for the mother to take it before or during pregnancy (pregnancy category X) and for a period after birth.[23]Methotrexate may increase the risk of certain cancers (lung cancer and melanoma for example), and the risk is believed to be higher for this drug than other disease-modifying anti-rheumatic drugs (DMARDS)).[24]
Central nervous system reactions to methotrexate have been reported, especially when given via the intrathecal route (directly into the cerebrospinal fluid), which include myelopathies and leucoencephalopathies. It has a variety of cutaneous side effects, particularly when administered in high doses.[25]
Another little understood but serious possible adverse effect of methotrexate is neurological damage and memory loss.[26] Neurotoxicity may result from the drug crossing the blood–brain barrier and damaging neurons in the cerebral cortex. People with cancer who receive the medication often nickname these effects "chemo brain" or "chemo fog".[26]
Drug interactions[edit]
Penicillins may decrease the elimination of methotrexate, so increase the risk of toxicity.[1] While they may be used together, increased monitoring is recommended.[1]The aminoglycosides, neomycin and paromomycin, have been found to reduce gastrointestinal (GI) absorption of methotrexate.[27] Probenecid inhibits methotrexate excretion, which increases the risk of methotrexate toxicity.[27] Likewise, retinoids and trimethoprim have been known to interact with methotrexate to produce additive hepatotoxicity and haematotoxicity, respectively.[27] Other immunosuppressants like ciclosporin may potentiate methotrexate's haematologic effects, hence potentially leading to toxicity.[27] NSAIDs have also been found to fatally interact with methotrexate in numerous case reports.[27] Nitrous oxide potentiating the haematological toxicity of methotrexate has also been documented.[27] Proton-pump inhibitors such as omeprazole and the anticonvulsant valproate have been found to increase the plasma concentrations of methotrexate, as have nephrotoxic agents such as cisplatin, the GI drug colestyramine, and dantrolene.[27]
Mechanism of action[edit]
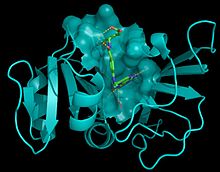
Methotrexate is an antimetabolite of the antifolate type. It is thought to affect cancer and rheumatoid arthritis by two different pathways. For cancer, methotrexate competitively inhibits dihydrofolate reductase (DHFR), an enzyme that participates in the tetrahydrofolate synthesis.[28][29] The affinity of methotrexate for DHFR is about 1000-fold that of folate. DHFR catalyses the conversion of dihydrofolate to the active tetrahydrofolate.[28] Folic acid is needed for the de novo synthesis of the nucleosidethymidine, required for DNA synthesis.[28] Also, folate is essential for purine and pyrimidine base biosynthesis, so synthesis will be inhibited. Methotrexate, therefore, inhibits the synthesis of DNA, RNA, thymidylates, and proteins.[28]
For the treatment of rheumatoid arthritis, inhibition of DHFR is not thought to be the main mechanism, but rather multiple mechanisms appear to be involved, including the inhibition of enzymes involved in purine metabolism, leading to accumulation of adenosine; inhibition of T cell activation and suppression of intercellular adhesion molecule expression by T cells; selective down-regulation of B cells; increasing CD95 sensitivity of activated T cells; and inhibition of methyltransferase activity, leading to deactivation of enzyme activity relevant to immune system function.[30][31] Another mechanism of MTX is the inhibition of the binding of interleukin 1-beta to its cell surface receptor.[32]
History[edit]
In 1947, a team of researchers led by Sidney Farber showed aminopterin, a chemical analogue of folic acid developed by Yellapragada Subbarao of Lederle, could induce remission in children with acute lymphoblastic leukemia. The development of folic acid analogues had been prompted by the discovery that the administration of folic acid worsened leukemia, and that a diet deficient in folic acid could, conversely, produce improvement; the mechanism of action behind these effects was still unknown at the time.[33] Other analogues of folic acid were in development, and by 1950, methotrexate (then known as amethopterin) was being proposed as a treatment for leukemia.[34] Animal studies published in 1956 showed the therapeutic index of methotrexate was better than that of aminopterin, and clinical use of aminopterin was thus abandoned in favor of methotrexate.
In 1951, Jane C. Wright demonstrated the use of methotrexate in solid tumors, showing remission in breast cancer.[35] Wright's group was the first to demonstrate use of the drug in solid tumors, as opposed to leukemias, which are a cancer of the marrow. Min Chiu Li and his collaborators then demonstrated complete remission in women with choriocarcinoma and chorioadenoma in 1956,[36] and in 1960 Wright et al. produced remissions in mycosis fungoides.[37][38]