Effect of low doses of estradiol and tamoxifen on breast cancer cell ...
Estradiol và tamoxifen kháng T47D
Estradiol
From Wikipedia, the free encyclopedia
 | |
 | |
| Names | |
|---|---|
| Pronunciation | /ˌɛstrəˈdaɪoʊl/ ES-trə-DYE-ohl[1][2] |
| IUPAC name
(8R,9S,13S,14S,17S)-13-Methyl-6,7,8,9,11,12,14,15,16,17-decahydrocyclopenta[a]phenanthrene-3,17-diol
| |
| Other names
Estra-1,3,5(10)-triene-3,17β-diol; 17β-Estradiol
| |
| Identifiers | |
3D model (JSmol)
| |
| ChEBI | |
| ChemSpider | |
| DrugBank | |
| ECHA InfoCard | 100.000.022 |
| KEGG | |
PubChem CID
| |
| UNII | |
| Properties | |
| C18H24O2 | |
| Molar mass | 272.38 g/mol |
| -186.6·10−6 cm3/mol | |
| Pharmacology | |
| G03CA03 (WHO) | |
| Oral, sublingual, intranasal, topical/transdermal, vaginal, intramuscular or subcutaneous (as an ester), subdermal implant | |
| Pharmacokinetics: | |
| Oral: <5%[3] | |
| ~98%:[3][4] • Albumin: 60% • SHBG: 38% • Free: 2% | |
| Liver (via hydroxylation, sulfation, glucuronidation) | |
| Oral: 13–20 hours[3] Sublingual: 8–18 hours[5] Topical (gel): 36.5 hours[6] | |
| Urine: 54%[3] Feces: 6%[3] | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
| Infobox references | |
Estradiol (E2), also spelled oestradiol, is a steroid, an estrogen, and the primary female sex hormone. It is named for and is important in the regulation of the estrous and menstrual female reproductive cycles. Estradiol is essential for the development and maintenance of female reproductive tissues such as the breasts, uterus, and vagina during puberty, adulthood, and pregnancy,[7] but it also has important effects in many other tissues including bone, fat, skin, liver, and the brain. While estrogen levels in men are lower compared to women, estrogens have essential functions in men as well. Estradiol is found in most vertebrates as well as many crustaceans, insects, fish, and other animal species.[8][9]
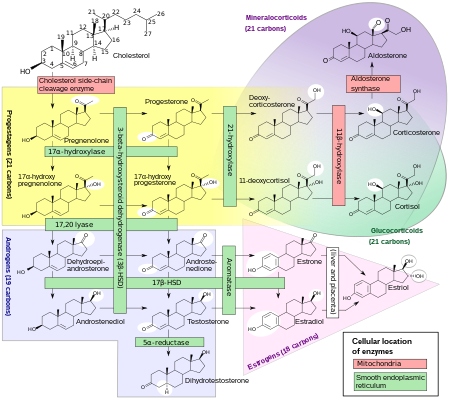
Estradiol is produced especially within the follicles of the female ovaries, but also in other endocrine (i.e., hormone-producing) and non-endocrine tissues (e.g., including fat, liver, adrenal, breast, and neural tissues). Estradiol is biosynthesized from cholesterol through a series of chemical intermediates.[10] One principal pathway involves the generation of 4-androstenedione, which is converted into estrone by aromatase and then by 17β-hydroxysteroid dehydrogenase into estradiol. Alternatively, 4-androstenedione can be converted into testosterone, an androgen and the primary male sex hormone, which in turn can be aromatized into estradiol.
Biological function[edit]
Sexual development[edit]
The development of secondary sex characteristics in women is driven by estrogens, to be specific, estradiol.[11][12] These changes are initiated at the time of puberty, most are enhanced during the reproductive years, and become less pronounced with declining estradiol support after menopause. Thus, estradiol produces breast development, and is responsible for changes in the body shape, affecting bones, joints, and fat deposition.[11][12] In females, estradiol induces breast development, widening of the hips, a feminine fat distribution (with fat deposited particularly in the breasts, hips, thighs, and buttocks), and maturation of the vagina and vulva, whereas it mediates the pubertal growth spurt (indirectly via increased growth hormone secretion)[13] and epiphyseal closure (thereby limiting final height) in both sexes.[11][12]
Reproduction[edit]
Female reproductive system[edit]
In the female, estradiol acts as a growth hormone for tissue of the reproductive organs, supporting the lining of the vagina, the cervical glands, the endometrium, and the lining of the fallopian tubes. It enhances growth of the myometrium. Estradiol appears necessary to maintain oocytes in the ovary. During the menstrual cycle, estradiol produced by the growing follicle triggers, via a positive feedback system, the hypothalamic-pituitary events that lead to the luteinizing hormone surge, inducing ovulation. In the luteal phase, estradiol, in conjunction with progesterone, prepares the endometrium for implantation. During pregnancy, estradiol increases due to placental production. The effect of estradiol, together with estrone and estriol, in pregnancy is less clear. They may promote uterine blood flow, myometrial growth, stimulate breast growth and at term, promote cervical softening and expression of myometrial oxytocinreceptors.[citation needed] In baboons, blocking of estrogen production leads to pregnancy loss, suggesting estradiol has a role in the maintenance of pregnancy. Research is investigating the role of estrogens in the process of initiation of labor. Actions of estradiol are required before the exposure of progesterone in the luteal phase.[citation needed]
Male reproductive system[edit]
The effect of estradiol (and estrogens in general) upon male reproduction is complex. Estradiol is produced by action of aromatase mainly in the Leydig cells of the mammalian testis, but also by some germ cells and the Sertoli cells of immature mammals.[14] It functions (in vitro) to prevent apoptosis of male sperm cells.[15] While some studies in the early 1990s claimed a connection between globally declining sperm counts and estrogen exposure in the environment,[16] later studies found no such connection, nor evidence of a general decline in sperm counts.[17][18] Suppression of estradiol production in a subpopulation of subfertile men may improve the semen analysis.[19]
Males with certain sex chromosome genetic conditions, such as Klinefelter's syndrome, will have a higher level of estradiol.[20]
Skeletal system[edit]
Estradiol has a profound effect on bone. Individuals without it (or other estrogens) will become tall and eunuchoid, as epiphyseal closure is delayed or may not take place. Bone structure is affected also, resulting in early osteopenia and osteoporosis.[21] Also, women past menopause experience an accelerated loss of bone mass due to a relative estrogen deficiency.[22]
Skin health[edit]
The estrogen receptor, as well as the progesterone receptor, have been detected in the skin, including in keratinocytes and fibroblasts.[23][24] At menopause and thereafter, decreased levels of female sex hormones result in atrophy, thinning, and increased wrinkling of the skin and a reduction in skin elasticity, firmness, and strength.[23][24] These skin changes constitute an acceleration in skin aging and are the result of decreased collagen content, irregularities in the morphology of epidermal skin cells, decreased ground substance between skin fibers, and reduced capillaries and blood flow.[23][24] The skin also becomes more dry during menopause, which is due to reduced skin hydration and surface lipids (sebum production).[23] Along with chronological aging and photoaging, estrogen deficiency in menopause is one of the three main factors that predominantly influences skin aging.[23]
HRT, consisting of systemic treatment with estrogen alone or in combination with a progestogen, has well-documented and considerable beneficial effects on the skin of postmenopausal women.[23][24] These benefits include increased skin collagen content, skin thickness and elasticity, and skin hydration and surface lipids.[23][24] Topical estrogen has been found to have similar beneficial effects on the skin.[23] In addition, a study has found that topical 2% progesterone cream significantly increases skin elasticity and firmness and observably decreases wrinkles in peri- and postmenopausal women.[24] Skin hydration and surface lipids, on the other hand, did not significantly change with topical progesterone.[24] These findings suggest that progesterone, like estrogen, also has beneficial effects on the skin, and may be independently protective against skin aging.[24]
Nervous system[edit]
Estrogens can be produced in the brain from steroid precursors. As antioxidants, they have been found to have neuroprotective function.[25]
The positive and negative feedback loops of the menstrual cycle involve ovarian estradiol as the link to the hypothalamic-pituitary system to regulate gonadotropins.[26](See Hypothalamic–pituitary–gonadal axis.)
Estrogen is considered to play a significant role in women’s mental health, with links suggested between the hormone level, mood and well-being. Sudden drops or fluctuations in, or long periods of sustained low levels of estrogen may be correlated with significant mood-lowering. Clinical recovery from depression postpartum, perimenopause, and postmenopause was shown to be effective after levels of estrogen were stabilized and/or restored.[27][28]
Recently, the volumes of sexually dimorphic brain structures in transgender women were found to change and approximate typical female brain structures when exposed to estrogen concomitantly with androgen deprivation over a period of months,[29] suggesting that estrogen and/or androgens have a significant part to play in sex differentiation of the brain, both prenatally and later in life.
There is also evidence the programming of adult male sexual behavior in many vertebrates is largely dependent on estradiol produced during prenatal life and early infancy.[30] It is not yet known whether this process plays a significant role in human sexual behavior, although evidence from other mammals tends to indicate a connection.[31]
Estrogen has been found to increase the secretion of oxytocin and to increase the expression of its receptor, the oxytocin receptor, in the brain.[32] In women, a single dose of estradiol has been found to be sufficient to increase circulating oxytocin concentrations.[33]
Gynecological cancers[edit]
Estradiol has been tied to the development and progression of cancers such as breast cancer, ovarian cancer and endometrial cancer. Estradiol affects target tissues mainly by interacting with two nuclear receptors called estrogen receptor α (ERα) and estrogen receptor β (ERβ).[34][35] One of the functions of these estrogen receptors is the modulation of gene expression. Once estradiol binds to the ERs, the receptor complexes then bind to specific DNA sequences, possibly causing damage to the DNA and an increase in cell division and DNA replication. Eukaryotic cells respond to damaged DNA by stimulating or impairing G1, S, or G2 phases of the cell cycle to initiate DNA repair. As a result, cellular transformation and cancer cell proliferation occurs.[36]
Other functions[edit]
Estradiol has complex effects on the liver. It affects the production of multiple proteins, including lipoproteins, binding proteins, and proteins responsible for blood clotting.[citation needed] In high amounts, estradiol can lead to cholestasis, for instance cholestasis of pregnancy.
Certain gynecological conditions are dependent on estrogen, such as endometriosis, leiomyomata uteri, and uterine bleeding.[citation needed]
Estrogen affects certain blood vessels. Improvement in arterial blood flow has been demonstrated in coronary arteries.[37]
Biological activity[edit]
Estradiol acts primarily as an agonist of the estrogen receptor (ER), a nuclear steroid hormone receptor. There are two subtypes of the ER, ERα and ERβ, and estradiol potently binds to and activates both of these receptors. The result of ER activation is a modulation of gene transcription and expression in ER-expressing cells, which is the predominant mechanism by which estradiol mediates its biological effects in the body. Estradiol also acts as an agonist of membrane estrogen receptors (mERs), such as GPER (GPR30), a recently discovered non-nuclear receptor for estradiol, via which it can mediate a variety of rapid, non-genomic effects.[38] Unlike the case of the ER, GPER appears to be selective for estradiol, and shows very low affinities for other endogenous estrogens, such as estrone and estriol.[39] Additional mERs besides GPER include ER-X, ERx, and Gq-mER.[40][41]
ERα/ERβ are in inactive state trapped in multimolecular chaperone complexes organized around the heat shock protein 90 (HSP90), containing p23 protein, and immunophilin, and located in majority in cytoplasm and partially in nucleus. In the E2 classical pathway or estrogen classical pathway, estradiol enters the cytoplasm, where it interacts with ERs. Once bound E2, ERs dissociate from the molecular chaperone complexes and become competent to dimerize, migrate to nucleus, and to bind to specific DNA sequences (estrogen response element, ERE), allowing for gene transcription which can take place over hours and days.
Estradiol is reported to be approximately 12 times as potent as estrone and 80 times as potent as estriol in its estrogenic activity.[42][43] As such, estradiol is the main estrogen in the body, although the roles of estrone and estriol as estrogens are said to not be negligible.[43]
Biochemistry[edit]
Biosynthesis[edit]
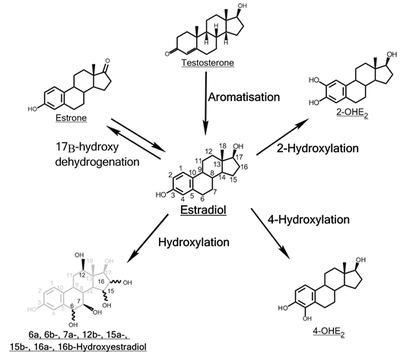
Estradiol, like other steroids, is derived from cholesterol. After side chain cleavage and using the Δ5 or the Δ4- pathway, Δ4-androstenedione is the key intermediary. A portion of the Δ4-androstenedione is converted to testosterone, which in turn undergoes conversion to estradiol by aromatase. In an alternative pathway, Δ4-androstenedione is aromatized to estrone, which is subsequently converted to estradiol.[45]
During the reproductive years, most estradiol in women is produced by the granulosa cells of the ovaries by the aromatization of Δ4-androstenedione (produced in the theca folliculi cells) to estrone, followed by conversion of estrone to estradiol by 17β-hydroxysteroid dehydrogenase. Smaller amounts of estradiol are also produced by the adrenal cortex, and, in men, by the testes.[citation needed]
Estradiol is not produced in the gonads only, in particular, fat cells produce active precursors to estradiol, and will continue to do so even after menopause.[46] Estradiol is also produced in the brain and in arterial walls.
The biosynthesis of estradiol-like compounds has been observed in leguminous plants, such as Phaseolus vulgaris and soybeans.[relevant? ][47] where they are termed phytoestrogens. Thus, consumption may have oestrogenic effects. In light of this, consumption can be counterproductive to patients undergoing treatment for breast cancer, which usually includes depriving the cancer cells of estrogens.
Distribution[edit]
In plasma, estradiol is largely bound to SHBG, and also to albumin. Only a fraction of 2.21% (± 0.04%) is free and biologically active, the percentage remaining constant throughout the menstrual cycle.[48]
Metabolism[edit]
Inactivation of estradiol includes conversion to less-active estrogens, such as estrone and estriol. Estriol is the major urinary metabolite.[citation needed] Estradiol is conjugated in the liver to form estrogen conjugates like estradiol sulfate, estradiol glucuronide and, as such, excreted via the kidneys. Some of the water-soluble conjugates are excreted via the bile duct, and partly reabsorbed after hydrolysis from the intestinal tract. This enterohepatic circulation contributes to maintaining estradiol levels.
Estradiol is also metabolized via hydroxylation into catechol estrogens. In the liver, it is non-specifically metabolized by CYP1A2, CYP3A4, and CYP2C9 via 2-hydroxylation into 2-hydroxyestradiol, and by CYP2C9, CYP2C19, and CYP2C8 via 17β-hydroxy dehydrogenation into estrone,[49] with various other cytochrome P450 (CYP) enzymes and metabolic transformationsalso being involved.[50]
Estradiol is additionally esterified into lipoidal estradiol forms like estradiol palmitate and estradiol stearate to a certain extent; these esters are stored in adipose tissue and may act as a very long-lasting reservoir of estradiol.[51][52]
Levels[edit]
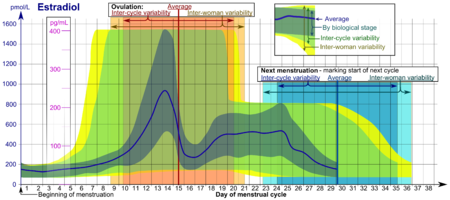
Levels of estradiol in premenopausal women are highly variable throughout the menstrual cycle and reference ranges widely vary from source to source.[53] Estradiol levels are minimal and according to most laboratories range from 20 to 80 pg/mL during the early to mid follicular phase (or the first week of the menstrual cycle, also known as menses).[54][55] Levels of estradiol gradually increase during this time and through the mid to late follicular phase (or the second week of the menstrual cycle) until the pre-ovulatory phase.[53][54] At the time of pre-ovulation (a period of about 24 to 48 hours), estradiol levels briefly surge and reach their highest concentrations of any other time during the menstrual cycle.[53] Circulating levels are typically between 130 and 200 pg/mL at this time, but in some women may be as high as 300 to 400 pg/mL, and the upper limit of the reference range of some laboratories are even greater (for instance, 750 pg/mL).[53][54][56][57][58] Following ovulation (or mid-cycle) and during the latter half of the menstrual cycle or the luteal phase, estradiol levels plateau and fluctuate between around 100 and 150 pg/mL during the early and mid luteal phase, and at the time of the late luteal phase, or a few days before menstruation, reach a low of around 40 pg/mL.[53][55] The mean integrated levels of estradiol during a full menstrual cycle have variously been reported by different sources as 80, 120, and 150 pg/mL.[55][59][60] Although contradictory reports exist, one study found mean integrated estradiol levels of 150 pg/mL in younger women whereas mean integrated levels ranged from 50 to 120 pg/mL in older women.[60]
During the reproductive years of the human female, levels of estradiol are somewhat higher than that of estrone, except during the early follicular phase of the menstrual cycle; thus, estradiol may be considered the predominant estrogen during human female reproductive years in terms of absolute serum levels and estrogenic activity.[citation needed] During pregnancy, estriol becomes the predominant circulating estrogen, and this is the only time at which estetrol occurs in the body, while during menopause, estrone predominates (both based on serum levels).[citation needed] The estradiol produced by male humans, from testosterone, is present at serum levels roughly comparable to those of postmenopausal women (14-55 versus <35 pg/mL, respectively).[citation needed] It has also been reported that if concentrations of estradiol in a 70-year-old man are compared to those of a 70-year-old woman, levels are approximately 2- to 4-fold higher in the man.[61]
Measurement[edit]
In women, serum estradiol is measured in a clinical laboratory and reflects primarily the activity of the ovaries. As such, they are useful in the detection of baseline estrogen in women with amenorrhea or menstrual dysfunction, and to detect the state of hypoestrogenicity and menopause. Furthermore, estrogen monitoring during fertility therapy assesses follicular growth and is useful in monitoring the treatment. Estrogen-producing tumors will demonstrate persistent high levels of estradiol and other estrogens. In precocious puberty, estradiol levels are inappropriately increased.
Ranges[edit]
Individual laboratory results should always been interpreted using the ranges provided by the laboratory that performed the test.
| Reference ranges for serum estradiol | |||
|---|---|---|---|
| Patient type | Lower limit | Upper limit | Unit |
| Adult male | 50[63] | 200[63] | pmol/L |
| 14 | 55 | pg/mL | |
| Adult female (follicular phase, day 5) | 70[63] 95% PI (standard) | 500[63] 95% PI | pmol/L |
| 110[64] 90% PI (used in diagram) | 220[64] 90% PI | ||
| 19 (95% PI) | 140 (95% PI) | pg/mL | |
| 30 (90% PI) | 60 (90% PI) | ||
| Adult female (preovulatory peak) | 400[63] | 1500[63] | pmol/L |
| 110 | 410 | pg/mL | |
| Adult female (luteal phase) | 70[63] | 600[63] | pmol/L |
| 19 | 160 | pg/mL | |
| Adult female - free (not protein bound) | 0.5[65][original research?] | 9[65][original research?] | pg/mL |
| 1.7[65][original research?] | 33[65][original research?] | pmol/L | |
| Post-menopausal female | N/A[63] | < 130[63] | pmol/L |
| N/A | < 35 | pg/mL | |
In the normal menstrual cycle, estradiol levels measure typically <50 pg/ml at menstruation, rise with follicular development (peak: 200 pg/ml), drop briefly at ovulation, and rise again during the luteal phase for a second peak. At the end of the luteal phase, estradiol levels drop to their menstrual levels unless there is a pregnancy.
During pregnancy, estrogen levels, including estradiol, rise steadily toward term. The source of these estrogens is the placenta, which aromatizes prohormonesproduced in the fetal adrenal gland.
Medical uses[edit]
Chemistry[edit]
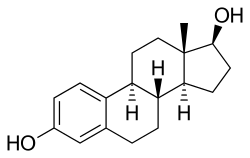
Estradiol is an estrane (C18) steroid.[66] It is also known as 17β-estradiol (to distinguish it from 17α-estradiol) or as estra-1,3,5(10)-triene-3,17β-diol. It has two hydroxyl groups, one at the C3 position and the other at the 17β position, as well as three double bonds in the A ring. Due to its two hydroxyl groups, estradiol is often abbreviated as E2. The structurally related estrogens, estrone (E1), estriol (E3), and estetrol (E4) have one, three, and four hydroxyl groups, respectively.
History[edit]
The discovery of estrogen is usually credited to the American scientists Edgar Allen and Edward A. Doisy.[67][68] In 1923, they observed that injection of fluid from porcine ovarian follicles produced pubertal- and estrus-type changes (including vaginal, uterine, and mammary gland changes and sexual receptivity) in sexually immature, ovariectomized mice and rats.[67][68][69] These findings demonstrated the existence of a hormone which is produced by the ovaries and is involved in sexual maturation and reproduction.[67][68][69] At the time of its discovery, Allen and Doisy did not name the hormone, and simply referred to it as an "ovarian hormone" or "follicular hormone";[68] others referred to it variously as feminin, folliculin, menformon, thelykinin, and emmenin.[70][71] In 1926, Parkes and Bellerby coined the term estrin to describe the hormone on the basis of it inducing estrus in animals.[72][70] Estrone was isolated and purified independently by Allen and Doisy and Germanscientist Adolf Butenandt in 1929, and estriol was isolated and purified by Marrian in 1930; they were the first estrogens to be identified.[68][73][74]
Estradiol, the most potent of the three major estrogens, was the last of the three to be identified.[68][72] It was discovered by Schwenk and Hildebrant in 1933, who synthesized it via reduction of estrone.[68] Estradiol was subsequently isolated and purified from sow ovaries by Doisy in 1935, with its chemical structure determined simultaneously,[75] and was referred to variously as dihydrotheelin, dihydrofolliculin, and dihydroxyestrin.[68][76] In 1935, the name estradiol and the term estrogen were formally established by the Sex Hormone Committee of the Health Organization of the League of Nations; this followed the names estrone (which was initially called theelin, progynon, folliculin, and ketohydroxyestrin) and estriol (initially called theelol and trihydroxyestrin) having been established in 1932 at the first meeting of the International Conference on the Standardization of Sex Hormones in London.[72][77] Following its discovery, a partial synthesis of estradiol from cholesterol was developed by Inhoffen and Hohlweg in 1940, and a total synthesis was developed by Anner and Miescher in 1948.[68]
In 1931, Butenandt found that the benzoic acid ester of estrone had a prolonged duration of action.[78][79] Subsequently, Schwenk and Hildebrant synthesized estradiol benzoate from estradiol in 1933,[80][81] and estradiol benzoate was introduced by Schering-Kahlbaum for medical use via intramuscular injection under the brand name Progynon-B in 1936.[82] It was the first estrogen ester to be marketed,[83] and has since been followed by many additional esters, for instance estradiol valerate and estradiol cypionate in the 1950s.[84][85][86] Ethinylestradiol was synthesized from estradiol by Inhoffen and Hohlweg in 1938 and was introduced for oral use by Schering in the United States under the brand name Estinyl in 1943.[80][87] It remains widely used in combined oral contraceptives.[80]
Society and culture[edit]
Etymology[edit]
The name estradiol derives from estra-, Gk. οἶστρος (oistros, literally meaning "verve or inspiration"),[88] which refers to the estrane steroid ring system, and -diol, a chemical term and suffix indicating that the compound is a type of alcohol bearing two hydroxyl groups.
Tamoxifen
From Wikipedia, the free encyclopedia
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Nolvadex, Genox, Tamifen, others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682414 |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 99% |
| Metabolism | Hepatic (CYP3A4, 2C9 and 2D6) |
| Biological half-life | 5-7 days[2] |
| Excretion | Faeces (65%), urine (9%) |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.031.004 |
| Chemical and physical data | |
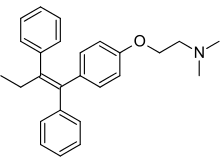
| Formula | C26H29NO |
| Molar mass | 371.515 g/mol 563.638 g/mol (citrate salt) |
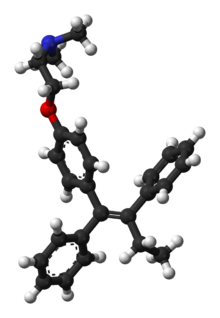
| 3D model (Jmol) | |
| (verify) | |
Tamoxifen (TMX), sold under the brand name Nolvadex among others, is a medication that is used to prevent breast cancer in women and treat breast cancer in women and men.[3] It is also being studied for other types of cancer.[3] It has been used for Albright syndrome. Tamoxifen is typically taken daily by mouth for five years for breast cancer.[4]
Serious side effects include a small increased risk of uterine cancer, stroke, vision problems, and pulmonary embolism. Common side effects include irregular periods, weight loss, and hot flashes. It may cause harm to the baby if taken during pregnancy or breastfeeding.[4] It is a selective estrogen-receptor modulator (SERM) that works both by decreasing factors that increase the growth of breast cells and increasing factors that decrease the growth of breast cells.[4][5] It is of the triphenylethylene group.[6]
Tamoxifen was discovered in 1967.[7] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[8] Tamoxifen is available as a generic medication.[4] The wholesale price in the developing world is about 0.07 to 0.23 USD per day.[9] In the United States it costs about 2 USD a day.[4]
Contents
[hide]Medical uses[edit]
Breast cancer[edit]
Tamoxifen is currently used for the treatment of both early and advanced estrogen receptor (ER)-positive (ER+) breast cancer in pre- and post-menopausal women.[10] Additionally, it is the most common hormone treatment for male breast cancer.[11] It is also approved by the FDA for the prevention of breast cancer in women at high risk of developing the disease.[12] It has been further approved for the reduction of contralateral (in the opposite breast) cancer. The use of tamoxifen is recommended for 10 years.[13]
In 2006, the large STAR clinical study concluded that raloxifene is equally effective in reducing the incidence of breast cancer, but after an average 4-year follow-up there were 36% fewer uterine cancers and 29% fewer blood clots in women taking raloxifene than in women taking tamoxifen, although the difference was not statistically significant.[14][15][16]
Infertility[edit]
Tamoxifen is used to treat infertility in women with anovulatory disorders. It is given at days 3–7 of a woman's cycle.[17]
Tamoxifen improves fertility in males with infertility by disinhibiting the hypothalamic-pituitary-adrenal axis (via ER antagonism) and thereby increasing the secretion of luteinizing hormone and follicle-stimulating hormone and increasing testicular testosterone production.[18]
Gynecomastia[edit]
Tamoxifen is used to prevent estrogen-related gynecomastia, resulting from elevated estrogenic levels. It is taken as a preventative measure in small doses, or used at the onset of any symptoms such as nipple soreness or sensitivity. Other drugs are taken for similar purposes such as clomiphene citrate and the anti-aromatase drugs which are used in order to try to avoid the hormone-related adverse effects. Tamoxifen is also sometimes used to treat or prevent gynecomastia in sex offenders undergoing temporary chemical castration.[19]
Others[edit]
Occasionally tamoxifen is used in treatment of the rare conditions of retroperitoneal fibrosis[20] and idiopathic sclerosing mesenteritis.[21]
Side effects[edit]
A report in September 2009 from Health and Human Services' Agency for Healthcare Research and Quality suggests that tamoxifen, raloxifene, and tibolone used to treat breast cancer significantly reduce invasive breast cancer in midlife and older women, but also increase the risk of adverse side effects.[22]
Some cases of lower-limb lymphedema have been associated with the use of tamoxifen, due to the blood clots and deep vein thrombosis (DVT) that can be caused by this medication. Resolution of the blood clots or DVT is needed before lymphedema treatment can be initiated.
Bone[edit]
A beneficial side effect of tamoxifen is that it prevents bone loss by acting as an ER agonist (i.e., mimicking the effects of estrogen) in this cell type. Therefore, by inhibiting osteoclasts, it prevents osteoporosis.[23][24] When tamoxifen was launched as a drug, it was thought that tamoxifen would act as an ER antagonist in all tissue, including bone, and therefore it was feared that it would contribute to osteoporosis. It was therefore very surprising that the opposite effect was observed clinically. Hence tamoxifen's tissue selective action directly led to the formulation of the concept of SERMs.[25] In contrast tamoxifen appears to be associated with bone loss in premenopausal women who continue to menstruate after adjuvant chemotherapy.[26]
Endometrial cancer[edit]
Tamoxifen is a SERM.[27] Even though it is an antagonist in breast tissue it acts as partial agonist on the endometrium and has been linked to endometrial cancer in some women. Therefore, endometrial changes, including cancer, are among tamoxifen's side effects.[28] With time, risk of endometrial cancer may be doubled to quadrupled, which is a reason tamoxifen is typically only used for 5 years.[29]
The American Cancer Society lists tamoxifen as a known carcinogen, stating that it increases the risk of some types of uterine cancer while lowering the risk of breast cancer recurrence.[30] The ACS states that its use should not be avoided in cases where the risk of breast cancer recurrence without the drug is higher than the risk of developing uterine cancer with the drug.
Cardiovascular and metabolic[edit]
Tamoxifen treatment of postmenopausal women is associated with beneficial effects on serum lipid profiles. However, long-term data from clinical trials have failed to demonstrate a cardioprotective effect.[31] For some women, tamoxifen can cause a rapid increase in triglyceride concentration in the blood.[citation needed] In addition there is an increased risk of thromboembolism especially during and immediately after major surgery or periods of immobility.[32] Tamoxifen is also a cause of fatty liver, otherwise known as steatorrhoeic hepatosis or steatosis hepatis.[33]
Central nervous system[edit]
Tamoxifen-treated breast cancer patients show evidence of reduced cognition,[34] a major side effect of tamoxifen, and semantic memory scores.[35] However memory impairment in patients treated with tamoxifen was less severe compared with those treated with anastrozole (an aromatase inhibitor).[36]
A significant number of tamoxifen-treated breast cancer patients experience a reduction of libido.[37][38]
Premature growth plate fusion[edit]
While tamoxifen has been shown to antagonize the actions of estrogen in tissues such as the breast, its effects in other tissues such as bones has not been documented fully. There have been studies done in mice showing tamoxifen mimic the effects of estrogen on bone metabolism and skeletal growth. Thus increasing the possibility of pre-mature bone fusion. This effect would be less of a concern in adults who have stopped growing.[39]
Pharmacogenetics and drug interactions[edit]
Patients with variant forms of the gene CYP2D6 (also called simply 2D6) may not receive full benefit from tamoxifen because of too slow metabolism of the tamoxifen prodrug into its active metabolites.[40][41] On 18 October 2006, the Subcommittee for Clinical Pharmacology recommended relabeling tamoxifen to include information about this gene in the package insert.[42]
Certain CYP2D6 variations in breast cancer patients lead to a worse clinical outcome for tamoxifen treatment.[43] Genotypingtherefore has the potential for identification of women who have these CYP2D6 phenotypes and for whom the use of tamoxifen is associated with poor outcomes.
Recent studies suggest that taking the selective serotonin reuptake inhibitors (SSRIs) antidepressants paroxetine (Paxil), fluoxetine (Prozac), and sertraline (Zoloft) can decrease the effectiveness of tamoxifen, as these drugs compete for the CYP2D6 enzyme which is needed to metabolize tamoxifen into its active forms.[44] A U.S. study presented at the American Society of Clinical Oncology's annual meeting in 2009 found that after two years, 7.5% of women who took only tamoxifen had a recurrence, compared with 16% who took either paroxetine, fluoxetine or sertraline, drugs considered to be the most potent CYP2D6 inhibitors. That difference translates to a 120% increase in the risk of breast cancer recurrence. Patients taking the SSRIs; Celexa (citalopram), Lexapro (escitalopram), and Luvox (fluvoxamine), did not have an increased risk of recurrence, due to their lack of competitive metabolism for the CYP2D6 enzyme.[45] A newer study demonstrated a clearer and stronger effect from paroxetine in causing the worst outcomes. Patients treated with both paroxetine and tamoxifen have a 67% increased risk of death from breast cancer, from 24% to 91%, depending on the duration of coadministration.[46]
Recent research has shown that 7–10% of women with breast cancer may not receive the full medical benefit from taking tamoxifen due to their unique genetic make-up. DNA Drug Safety Testing can examine DNA variations in the CYP2D6 and other important drug processing pathways. More than 20% of all clinically used medications are metabolized by CYP2D6 and knowing the CYP2D6 status of a person can help the doctor with the future selection of medications.[47] Other molecular biomarkers may also be used to select appropriate patients likely to benefit from tamoxifen.[48]
Mechanism of action[edit]
Tamoxifen itself is a prodrug, having relatively little affinity for its target protein, the estrogen receptor (ER). It is metabolized in the liver by the cytochrome P450 isoform CYP2D6 and CYP3A4 into active metabolites such as 4-hydroxytamoxifen (4-OHT) (afimoxifene) and N-desmethyl-4-hydroxytamoxifen (endoxifen)[50] which have 30–100 times more affinity with the ER than tamoxifen itself.[51] These active metabolites compete with estrogen in the body for binding to the ER. In breast tissue, 4-OHT acts as an ER antagonist so that transcription of estrogen-responsive genes is inhibited.[52] Tamoxifen has 7% and 6% of the affinity of estradiol for the ERα and ERβ, respectively, whereas 4-OHT has 178% and 338% of the affinity of estradiol for the ERα and ERβ.[53]
4-OHT binds to ER, the ER/tamoxifen complex recruits other proteins known as co-repressors and then binds to DNA to modulate gene expression. Some of these proteins include NCoR and SMRT.[54] Tamoxifen function can be regulated by a number of different variables including growth factors.[55] Tamoxifen needs to block growth factor proteins such as ErbB2/HER2[56] because high levels of ErbB2 have been shown to occur in tamoxifen resistant cancers.[57] Tamoxifen seems to require a protein PAX2 for its full anticancer effect.[56][58] In the presence of high PAX2 expression, the tamoxifen/ER complex is able to suppress the expression of the pro-proliferative ERBB2 protein. In contrast, when AIB-1 expression is higher than PAX2, tamoxifen/ER complex upregulates the expression of ERBB2 resulting in stimulation of breast cancer growth.[56][59]
4-OHT binds to ER competitively (with respect to the endogenous agonist estrogen) in tumor cells and other tissue targets, producing a nuclear complex that decreases DNA synthesis and inhibits estrogen effects. It is a nonsteroidal agent with potent antiestrogenic properties which compete with estrogen for binding sites in breast and other tissues. Tamoxifen causes cells to remain in the G0 and G1 phases of the cell cycle. Because it prevents (pre)cancerous cells from dividing but does not cause cell death, tamoxifen is cytostatic rather than cytocidal.
The scientific literature is complex with respect to the activity of tamoxifen, and care should be taken to establish whether tamoxifen, or the 4-hydroxy metabolite was used, especially in in vitro assays.
N,N-Didesmethyl-4-hydroxytamoxifen (norendoxifen), another active metabolite of tamoxifen, has been found to act as a potent competitive aromatase inhibitor (IC50 = 90 nM), and may also be involved in its antiestrogenic activity.[60]
History[edit]
In the late 1950s, pharmaceutical companies were actively researching a newly discovered class of anti-estrogen compounds in the hope of developing a morning-after contraceptive pill. Arthur L Walpole was a reproductive endocrinologist who led such a team at the Alderley Park research laboratories of ICI Pharmaceuticals. It was there in 1966 that Dora Richardson first synthesised tamoxifen, known then as ICI-46,474.[61] Walpole and his colleagues filed a UK patent covering this compound in 1962, but patent protection on this compound was repeatedly denied in the US until the 1980s.[62] Tamoxifen did eventually receive marketing approval as a fertility treatment, but the class of compounds never proved useful in human contraception. A link between estrogen and breast cancer had been known for many years, but cancer treatments were not a corporate priority at the time, and Walpole's personal interests were important in keeping support for the compound alive in the face of this and the lack of patent protection.[7]
Tamoxifen is one of three drugs in an anti-angiogenetic protocol developed by Dr. Judah Folkman, a researcher at Children's Hospital at Harvard Medical School in Boston. Folkman discovered in the 1970s that angiogenesis – the growth of new blood vessels – plays a significant role in the development of cancer. Since his discovery, an entirely new field of cancer research has developed. Clinical trials on angiogenesis inhibitors have been underway since 1992 using myriad different drugs. The Harvard researchers developed a specific protocol for a golden retriever named Navy who was cancer-free after receiving the prescribed cocktail of celecoxib, doxycycline, and tamoxifen – the treatment subsequently became known as the Navy Protocol.[63] Furthermore, tamoxifen treatment alone has been shown to have anti-angiogenetic effects in animal models of cancer which appear to be, at least in part, independent of tamoxifen's ER antagonist properties.[64]
The first clinical study took place at the Christie Hospital in 1971, and showed a convincing effect in advanced breast cancer,[65] but nevertheless ICI's development programme came close to termination when it was reviewed in 1972. Tamoxifen's further development may have been bolstered by a second clinical study by Harold W.C. Ward [66] at the Queen Elizabeth Hospital, Birmingham. Ward's study showed a more definitive response to the drug at a higher dosage. Walpole also may have helped to convince the company to market tamoxifen for late stage breast cancer in 1973.[62] He was also instrumental in funding V. Craig Jordan to work on tamoxifen. In 1972, ICI Pharmaceuticals Division abandoned development of tamoxifen for financial reasons. The drug was subsequently reinvented from a failed contraceptive, to become tamoxifen, the gold standard for the adjuvant treatment of breast cancer and the pioneering medicine for chemprevention for high risk women.[67][68] Two books, Estrogen Action, Selective Estrogen Receptor Modulators and Women's Health (Imperial College Press 2013) and Tamoxifen Pioneering Medicine in Breast Cancer (Springer 2013) tell this story.
1980 saw the publication of the first trial to show that tamoxifen given in addition to chemotherapy improved survival for patients with early breast cancer.[69] In advanced disease, tamoxifen is now only recognized as effective in ER+ patients, but the early trials did not select ER+ patients, and by the mid 1980s the clinical trial picture was not showing a major advantage for tamoxifen.[70] Nevertheless, tamoxifen had a relatively mild side-effect profile, and a number of large trials continued.
The pharmacology of SERMs was discovered, defined, and deciphered during the 1980s [71] A clinical strategy was described [72] that led to the creation of SERMs as a group of multifunctional medicines aimed at the treatment or prevention of many conditions in postmenopausal women, e.g.: osteoporosis and breast cancer. This story is told in: V. Craig Jordan, ed. 2013. "Estrogen Action, Selective Estrogen Receptor Modulators and Women's Health" Imperial College Press, Singapore.
It was not until 1998 that the meta-analysis of the Oxford-based Early Breast Cancer Trialists' Collaborative Group showed definitively that tamoxifen saved lives in early breast cancer.[73]
Society and culture[edit]
Economics[edit]
Global sales of tamoxifen in 2001 were $1,024 million.[74] Since the expiration of the patent in 2002, it is now widely available as a generic drug around the world. As of 2004, tamoxifen was the world's largest selling hormonal drug for the treatment of breast cancer.[75]
Research[edit]
Tamoxifen is used as a research tool to trigger tissue-specific gene expression in many conditional expression constructs in genetically modified animals including a version of the Cre-Lox recombination technique.[76]
The drug has also been studied in several additional indications.
Riedel's thyroiditis[edit]
Tamoxifen has been proposed as part of a treatment plan for Riedel's thyroiditis.[77]
Bipolar disorder[edit]
Tamoxifen has been shown to be effective in the treatment of mania in patients with bipolar disorder by blocking protein kinase C (PKC), an enzyme that regulates neuron activity in the brain. Researchers believe PKC is over-active during the mania in bipolar patients.[78][79]
McCune-Albright syndrome[edit]
In McCune-Albright syndrome (MAS) tamoxifen has been used to treat premature puberty and the consequences of premature puberty. Tamoxifen has been seen to decrease rapid bone maturation which is the result of excessive estrogen and alter predicted adult height (PAH).[80][81] The same effects have also been seen in short pubertal boys.[82]
However, one in vitro study in 2007 and later an in vivo study in 2008 have shown that tamoxifen induces apoptosis in growth plate chondrocytes, reduces serum IGF-Ilevels and causes persistent retardation of longitudinal and cortical radial bone growth in young male rats, leading the researches to express concern giving tamoxifen to growing individuals.[39][83]


No comments:
Post a Comment